Case Presentation:
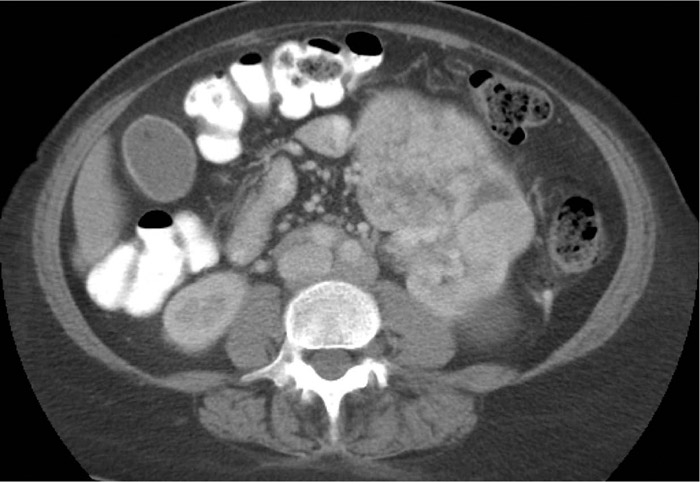
A 64‐year‐old woman presented with one month of intermittent epigastric abdominal discomfort and loose stools. She also noted a 7‐pound weight loss, poor appetite, fatigue, low‐grade fevers, sweats, dyspnea on exertion, aching bilateral calf cramps, and foot paresthesias. She endorsed occasional alcohol intake but denied tobacco or illicit substance use. Examination revealed pallor, epigastric fullness with mild tenderness to palpation, and diminished sensation in the bilateral plantar surfaces. Laboratory results included a white blood cell count of 3.6 x 103/μL, hemoglobin 7.5 g/dL with previous value 13.5 g/dL one year before, and alkaline phosphatase 275 IU/L. Erythrocyte sedimentation rate (ESR) was 110 mm/h. The peripheral blood smear demonstrated rouleaux and occasional spherocytes. Serum protein electrophoresis and immunofixation revealed an immunoglobulin M (IgM) kappa monoclonal gammopathy. Plasma viscosity was 2.18 centipoise. CT of the abdomen and pelvis demonstrated a 12.0 x 8.3 cm exophytic left renal mass, 16 cm splenomegaly, and retroperitoneal lymphadenopathy (see Fig 1). While awaiting lymph node biopsy, she was noted to have worsening lower extremity pain and progressive pancytopenia with hemolysis. Additional findings of hyperuricemia and renal insufficiency were thought to be due to tumor lysis syndrome and heme pigment nephropathy. She was treated with IV fluids, rasburicase, and corticosteroids. Skeletal survey was unremarkable. Bone marrow biopsy revealed 50% atypical lymphoplasmacytic cells with stains negative for amyloidosis. She received chemotherapy for Waldenström’s macroglobulinemia (WM) with rapid improvement. She refused further invasive testing. Repeat cross‐sectional imaging of the kidney mass is pending.
Discussion:
WM is a rare neoplasm of lymphoplasmacytoid cells that secrete monoclonal IgM. Clinical manifestations are numerous and result from both cellular infiltration of tissues (e.g. pancytopenia, constitutional symptoms, organomegaly) and IgM effects (e.g. hyperviscosity, peripheral neuropathy, leg cramps, autoimmune hemolytic anemia). Abdominal pain and loose stools have been described and are due to organomegaly and deposition of protein and cells into gastrointestinal tissues. Loss of erythrocyte electrostatic repulsion due to paraprotein leads to formation of rouleaux, which resembles a stack of coins. This finding has a wide differential diagnosis and leads to an elevated ESR. Case reports describe patients with kidney masses or giant kidneys as initial manifestations of WM. Rituximab combined with chemotherapy is the mainstay of therapy for advanced disease, and plasmapheresis is used for hyperviscosity.
Conclusions:
Hospitalists should consider WM in the differential diagnosis of multi‐system abnormalities, especially in those patients with rouleaux. This case highlights common and less common manifestations of this disorder, the two mechanisms of tissue injury, and the pattern recognition skills required for its prompt diagnosis.