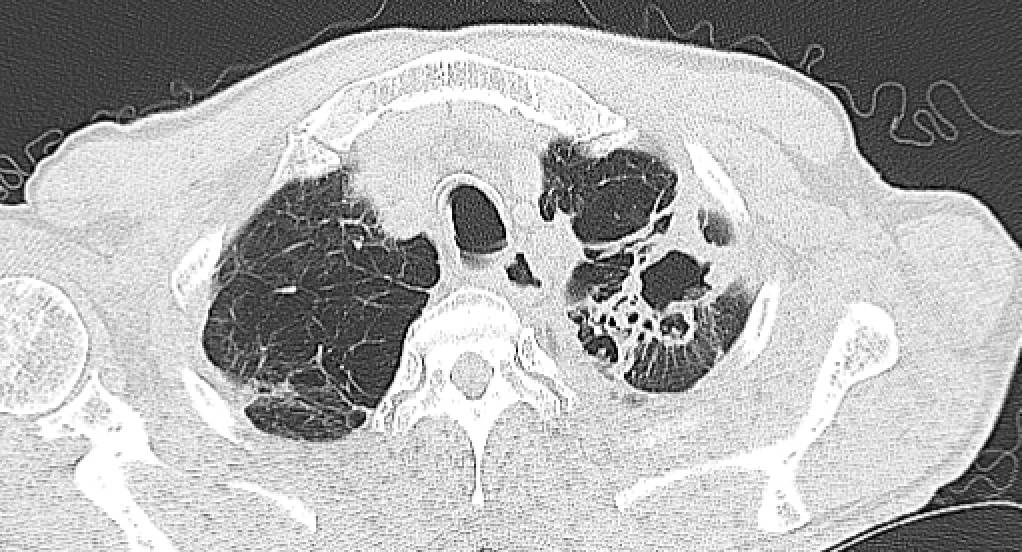
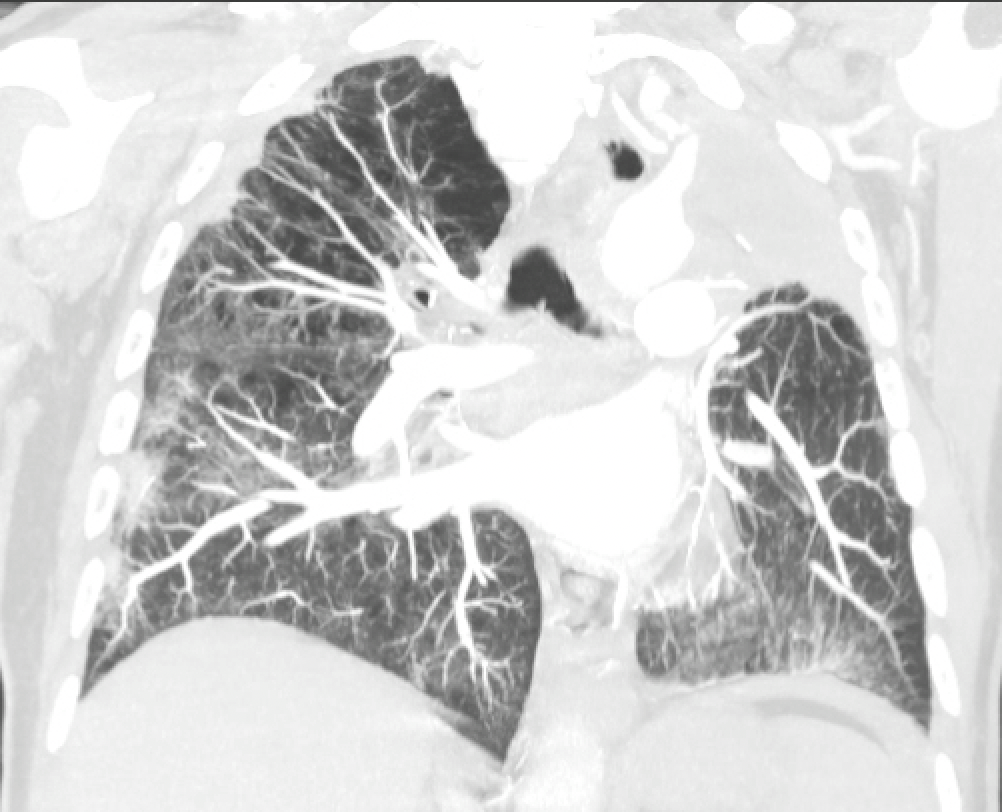
Case Presentation: A 68-year-old male with a history of heavy cigarette smoking and COPD presented with a six-month-long hacking cough with sputum production, night sweats, weight loss, and malaise. He was treated with multiple courses of azithromycin for community-acquired pneumonia without improvement. He had a history of asbestos exposure as a shipyard worker. He did not travel outside of the US and had no known exposure to TB. Imaging of the chest revealed a complex left upper lobe cavitary lesion with surrounding consolidation and nodular densities in the left upper and lower lobes with background emphysematous changes. He underwent bronchoscopy due to concerns of lung cancer. Bronchoalveolar lavage cultures later grew M. shimoidei, identified based on gene sequence analysis. Sputum was positive for acid-fast-bacilli and cultures also grew M. shimoidei. He was started on clarithromycin, rifabutin, and ethambutol. He had mild side effects of treatment, including nausea, fatigue, hair loss, and dry skin, but he managed to continue therapy. Cultures showed sensitivity to ethambutol and rifabutin but resistance to clarithromycin. On 6-month follow-up, he continued to have persistent low-grade fever and cough with purulent sputum speckled with black particulate matter. COPD symptoms had worsened, causing persistent wheezing and shortness of breath. Repeat CT of the chest showed progression in the size of the cavitary lesion with surrounding ground glass opacities. It was deemed that the antibiotic treatment had failed. After multidisciplinary discussion with pulmonary, infectious disease and cardiothoracic surgery teams, a decision was made to proceed with left upper lobectomy. The patient’s recovery was without any complications, and his symptoms improved significantly. Pathology of the resected specimen showed non-caseating granulomatous inflammation. On follow-up visits over the next 5 years, he remained symptom-free, and repeat sputum AFB tests continued to be negative. CT scans of the chest showed no recurrence of disease.
Discussion: Mycobacterium shimoidei is a rare, slow-growing nontuberculous mycobacterium, first isolated in Japan in 1968. Only one case was reported in the United States, out of a total of fifteen cases reported worldwide. Due to its rarity and the current understanding of its pathogenicity, identifying predisposing risk factors and providing effective treatment is limited. The infectious presentation is similar to TB, and it predominantly causes pulmonary disease. However, renal complications have also been reported. There is no current consensus on established therapy, but the triple-drug regimen, including clarithromycin, rifabutin, and ethambutol, has been effective in most reported cases. Additionally, Moxifloxacin and Levofloxacin, Sulfamethoxazole, Pyrazinamide, as well as Clofazimine have been reported to be potentially useful. There is limited experience with cases of macrolide resistance and therapeutic failure. There have never been any case reports requiring surgical resection which might be a potentially curative option for appropriately screened patients.
Conclusions: There are limited guidelines for treating M. shimoidei infection with drug resistance. Due to their extreme rarity, our knowledge is limited on surgical options for such cases with antibiotic failure. Our case highlights that surgical resection might be a curative option after a careful joint decision-making process among patients and multidisciplinary teams.