Background: There have been increases in the incidence of and significant costs associated with hospitalizations due to injection-related infection sequelae both in the U.S. and worldwide. Infection sequelae include but are not limited to cellulitis and abscess, bacteremia and sepsis, endocarditis, osteomyelitis, septic arthritis, ulcers, and thrombophlebitis. Because of the unique bio-socio-psycho needs of injection drug users, hospitalizations due to injection-related infection sequelae often contribute to increased length of stay, readmission rate, and expenses out of state and federal health care funding.
Methods: Interviews were conducted involving the key stakeholders in the patient care and care coordination. Interviewees include hospitalists, infectious disease specialists, nursing providers, care management specialists, mental health providers and primary care physicians. Through a pre-designed interview guide, interviewees were asked six questions focusing on: patient flow and process, challenges of providing care while in hospital, challenges in discharge process, challenges for outpatient follow ups, suggestions for improvement and data availability. Care processes and decision points were then mapped. Each stakeholder’s consideration, decision options, and resources constraints were outlined and summarized.
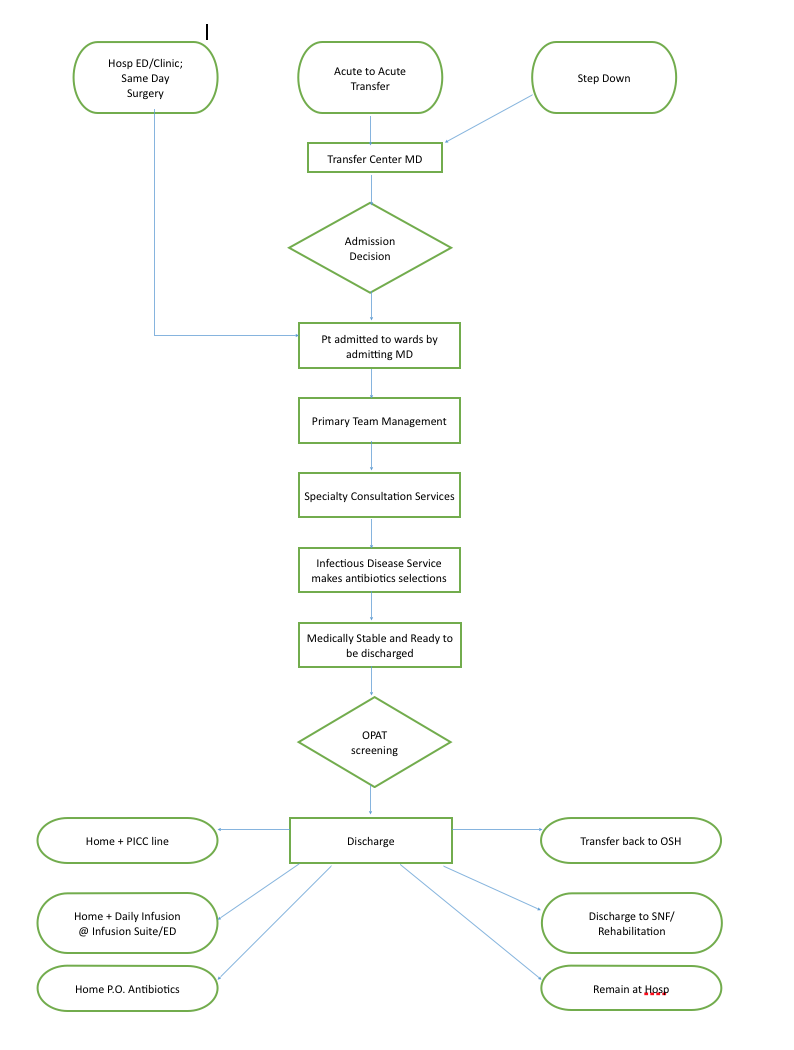
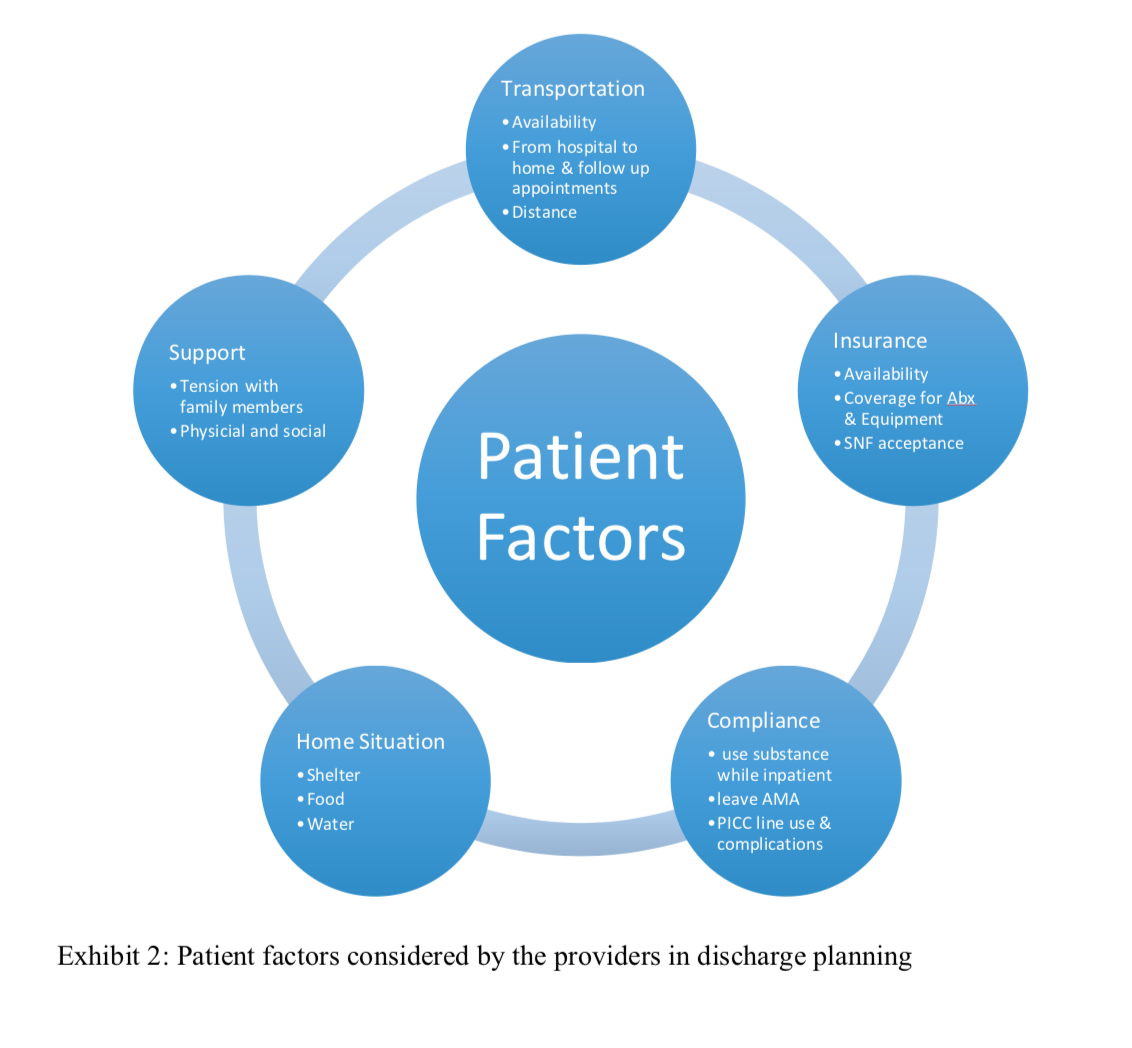
Results: Three key processes take place in the tertiary care setting for hospitalized IVDU patients due to injection-related infective sequelae include admission, clinical care, and discharge. Each phase involves multiple decision makings by key stakeholders. The diagram (Graph 1) provides a summary regarding the patient flow.The challenges of providing care to IVDU patients with infective sequelae were revealed in three aspects: patient factors, provider/care team factors, as well as system factors. It is agreeable among all the providers that the patient factors have the most significant influence in making the care process challenging and difficult.
Conclusions: Despite the fact that patient factors delay the discharge process the most, this study found the lacking of appropriate care facilities with drug rehabilitation capacity in subacute or community setting also significantly delayed the discharge process. The deficiency in care facilities manifested in gross availability as well as relative geographic distribution. While in hospital, the tension between care team members and the patient was aggravated by lack of inpatient addiction treatment. At discharge, patients would need continuing antibiotics therapy, physical therapy, and rehabilitation. However due to the social/behavior and financial reasons, they were highly likely to be rejected by subacute or skilled nursing facilities. Challenges and opportunities exist in both hospital and health system levels to provide improved care for hospitalized injection drug users due to injection-related infection sequelae.