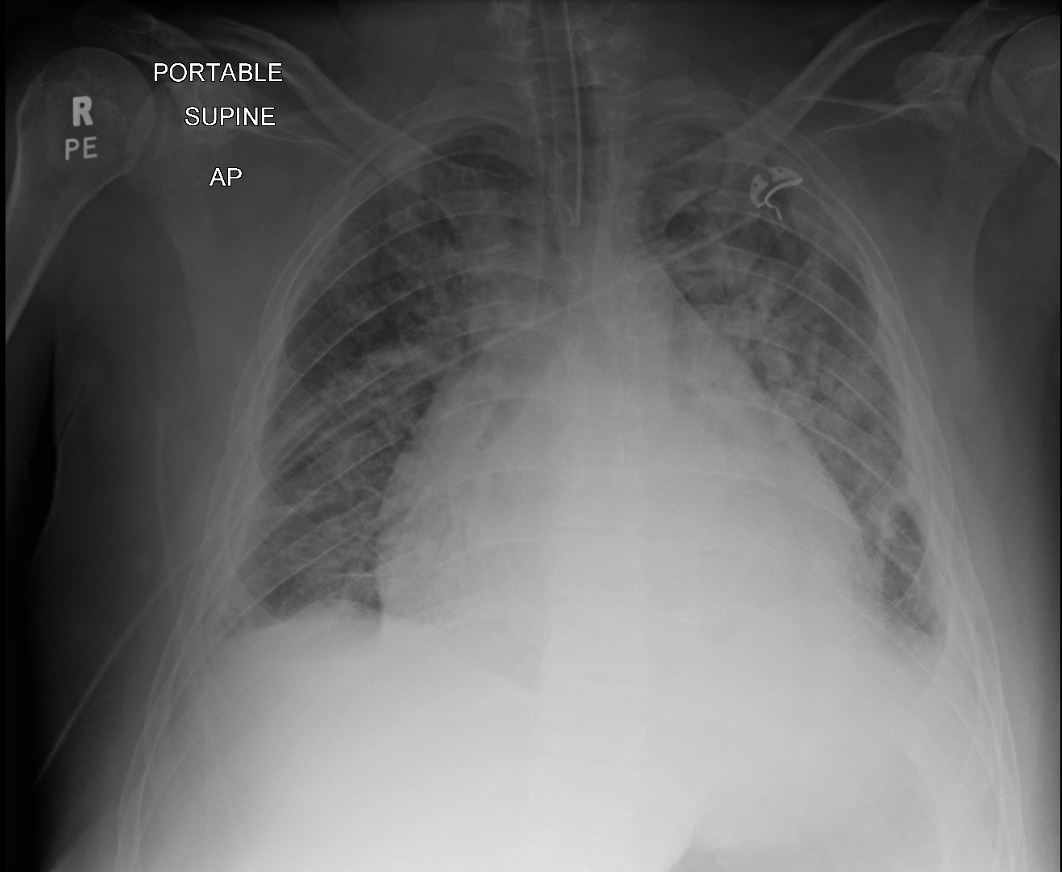
Case Presentation: A 26-year-old male presented to the ED with a 2 day history of shortness of breath, bilateral lower extremity edema, wet cough, and orthopnea. He reported a viral upper respiratory illness 1 prior, which resolved within 5 days with symptomatic management using Nyquil. On arrival, he was visibly dyspneic with vital signs showing HR 124 bpm, RR 32 breaths/min, BP 148/99 mmHg, and SpO₂ 79% on room air. During CT imaging, he experienced a seizure and was placed on a non-rebreather mask. Back in the ED, he developed pulseless electrical activity requiring 2 rounds of CPR, intubation, and sedation. Initial labs revealed hyponatremia (117 mmol/L), elevated creatinine (1.67 mg/dL), and BNP (1319 pg/mL). Urinalysis showed >100 mg/dL protein and large blood, with a urine microalbumin-creatinine ratio of 3277 mg/g. Chest X-ray revealed a prominent cardiac silhouette and patchy pulmonary opacities, while CTA confirmed diffuse interstitial infiltrates. Transthoracic echocardiography demonstrated a dilated left ventricle with an ejection fraction of 25-30%.Hyponatremia was managed with hypertonic saline, but worsening renal function necessitated dialysis. Serologic tests showed low C3/C4, ANA positivity, anti-dsDNA >300 IU/mL, and a p-ANCA titer of 1:20. Infectious studies revealed positive Coxsackievirus serologies and Mycoplasma pneumonia IgG. Renal biopsy confirmed class IV lupus nephritis. The diagnosis of systemic lupus erythematosus with viral myocarditis as a precipitating factor was made. Treatment included high-dose prednisone and mycophenolate mofetil, leading to symptomatic relief and improved cardiac function. The patient was discharged with a wearable defibrillator and scheduled for follow-up with nephrology, cardiology, and rheumatology teams.
Discussion: Systemic lupus erythematosus (SLE) is a complex autoimmune disease characterized by multi-organ involvement, often presenting with renal and cardiovascular complications. This case demonstrates how viral myocarditis can unmask latent SLE, culminating in lupus nephritis. Viral myocarditis, typically caused by agents like Coxsackievirus, can trigger immune dysregulation through mechanisms such as molecular mimicry and Toll-like receptor activation. In genetically predisposed individuals, this can lead to autoimmunity, as seen in this patient.Myocarditis in SLE is underrecognized due to nonspecific symptoms like dyspnea and fatigue. Advanced imaging, including cardiac MRI, is valuable for diagnosing myocardial inflammation. Diagnosing SLE amidst infection-related inflammation required comprehensive serologic evaluation and exclusion of infectious causes. Positive ANA and anti-dsDNA antibodies, hypocomplementemia, and biopsy findings confirmed the diagnosis. Management challenges included balancing immunosuppression to treat lupus nephritis while minimizing risks of viral reactivation.
Conclusions: This case underscores the importance of a multidisciplinary approach in managing overlapping autoimmune and infectious diseases. Immunosuppressive therapy targeted lupus nephritis while addressing myocarditis. This case highlights the need for clinicians to suspect underlying autoimmune conditions in young males with severe cardiac and renal involvement. Future research should explore biomarkers predicting autoimmune disease onset following viral infections.