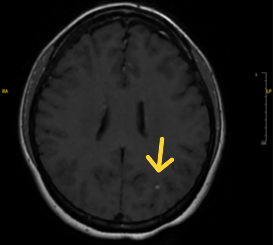
Case Presentation: A 38 year-old female with Crohn’s disease on infliximab presented to the ED with 3 weeks of fever, cough, and shortness of breath (SOB) unresponsive to a 10-day course of levofloxacin for presumed community acquired pneumonia (CAP). She emigrated from Ecuador in 2001 and was employed as a medical assistant in a private office. Chest X-ray revealed a patchy area of consolidation in the left upper lung. The fever, cough and SOB persisted despite empiric cefepime for suspected resistant CAP. A chest computed tomography (CT) angiography demonstrated a large mediastinal mass involving the hilum and encasing the left upper lobe bronchus with associated post-obstructive pneumonia. A QuantiFERON Gold-TB test was newly positive and rare acid-fast bacilli (AFB) were found on sputum smear. Bronchoscopy and biopsy revealed granulomas, and moderate AFB on smear, which were positive for mycobacterium tuberculosis on PCR. The patient was discharged on rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) and infliximab was held. Twenty-five days later, she returned with recurrent fevers, abdominal pain, nausea and vomiting, and headache despite adherence to RIPE treatment. CT chest revealed increase in necrotic mass-like consolidation involving the left upper lobe and hilum with associated confluent, infiltrative lymphadenopathy. Brain magnetic resonance imaging (MRI) revealed a 3mm L occipital lobe focus of enhancement. Spinal fluid analysis was unremarkable. TB-associated immune reconstitution inflammatory syndrome (IRIS) was suspected and corticosteroids were initiated with clinical response. The patient was discharged with close Department of Health surveillance. Four months after diagnosis, she continues to endorse clinical improvement on an anti-tuberculosis regimen.
Discussion: In the United States, TB cases have been rising. Diagnosis can be challenging given the diverse presentation of disease. TB should be suspected in those with risk factors such as healthcare, residence in endemic regions, and immune compromise or immunosuppressive therapy who are not improving despite appropriate treatment. IRIS is an exaggerated inflammatory response to a pre-existing infection following recovery of immunologic function. It reflects inflammatory burden rather than progressive infection or treatment failure. Initially associated with persons with HIV after initiation of antiretroviral therapy, IRIS is increasingly recognized in other scenarios of immune reconstitution, including withdrawal from tumor necrosis factor alpha (TNF-α) inhibitors. IRIS can occur in two forms: “unmasking” which is a flare-up of an underlying, undiagnosed infection once the patient is able to mount an immune response and “paradoxical”which is a recrudescence of symptoms of a treated infection. Diagnosis of paradoxical IRIS requires exclusion of other potential causes of clinical worsening. Time to onset varies by risk factor and by medication half-life– typically 5-16 weeks after TNF-α inhibitor withdrawal. IRIS can be mild or life threatening. While there is no treatment standard, corticosteroid therapy appears to shorten hospitalization and reduce morbidity.
Conclusions: We share a case of TB masquerading as CAP complicated by paradoxical TB-IRIS in a patient with Crohn’s disease on infliximab. With growing indications for immune modulating treatments, providers are encouraged to keep a heightened suspicion for TB and the potential for IRIS to facilitate earlier diagnosis and optimize outcomes.