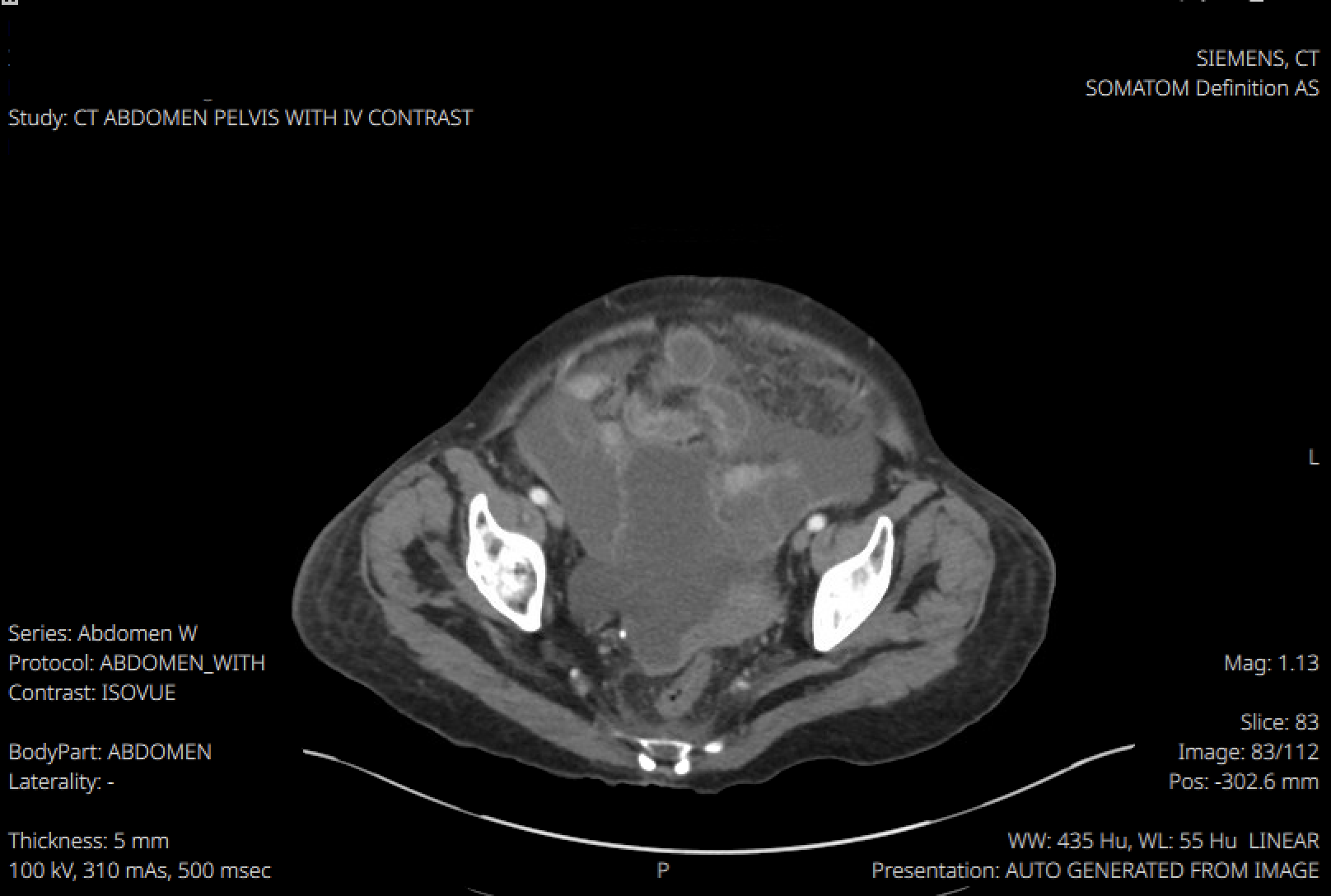
Case Presentation: FM was a 69-year-old female who immigrated from Mexico to the US 30 years ago with a history of primary biliary cholangitis complicated by cirrhosis, hepatic encephalopathy, and esophageal varices presented to the emergency department with worsening abdominal distension. She was a former smoker with no history of alcohol or recreational drug use. Her medical and family histories were negative for colitis, colon cancer, or irritable bowel disease. On admission, paracentesis showed SAAG 0.4, PMN 343, LDH 110, protein 3.7, and ADA 23 with no organism growth. Spontaneous bacterial peritonitis was presumed and FM started Ceftriaxone and albumin. A Transjugular Intrahepatic Portosystemic Shunt procedure was delayed due to infection. Repeat paracentesis showed SAAG 0.7 and PMN 399. With low SAAG, persistent ascites, a known left adnexal mass, and elevated CA125 and CA19-9, Gynecological Oncology was consulted. The absence of mass growth and normal inhibin B, AFP, and CEA made ovarian malignancy unlikely. After nine days with persistent symptoms, FM began trimethoprim sulfamethoxazole and underwent a TIPS procedure. The same day, a QuantiFERON GOLD test was strongly positive. Abdominal CT revealed omental caking and enlarged mediastinal lymph nodes, suggesting TB peritonitis. CT chest showed no pulmonary TB. After discharge, ascitic fluid cultures grew acid-fast bacilli confirmed as Mycobacterium tuberculosis via MTB probe. At follow up with Infectious Disease post-discharge, FM started RIPE therapy.
Discussion: FM’s clinical picture provides complex layered pathologies. A 12-year retrospective cohort study of 60 patients with peritoneal TB found that comorbidities such as cirrhosis, renal failure, diabetes, and malignancy significantly increased mortality risk [1]. FM’s pre-existing complicated PBC led clinicians to initially attribute her ascites to it. However, when presumed SBP treatment failed to resolve symptoms, the team investigated alternative causes, such as peritoneal TB and ovarian malignancy. A 2020 case study follows a 67-year-old woman with PBC and peritoneal TB, a rare dual diagnosis. While PBC is found with various autoimmune disorders, its association with TB is uncommon. The authors propose that the immunosuppressive state caused by PBC may increase TB susceptibility [2].Studies confirm that peritoneal TB can be fatal without timely diagnosis [1, 3]. No single diagnostic test is sufficient to rule it out. Chest radiograph and purified protein derivative (PPD) lack sensitivity. CT scan, smear tissue biopsy, and culture are the gold standard [3]. For FM, diagnostics included paracentesis, CT scans, malignancy workup, and an MTB analysis.FM’s paracentesis had neutrophilic predominance, often found in SBP, whereas peritoneal TB usually shows lymphocytic predominance. Persistent symptoms after antibiotic courses prompted further review. Her SAAG was < 1.1, excluding portal hypertension and suggesting malignancy, peritoneal TB, or pancreatitis. Ascitic fluid protein >2.5 excluded cirrhosis and pointed to malignancy, heart failure, or peritoneal TB.
Conclusions: FM’s case underscores the critical need for a broad differential diagnosis in patients with ascites, particularly in those with cirrhosis, where conditions like peritoneal TB, SBP, and malignancy may present with overlapping clinical features. This case reinforces the importance of comprehensive analysis of ascitic fluid parameters and vigilance for atypical causes such as peritoneal TB.