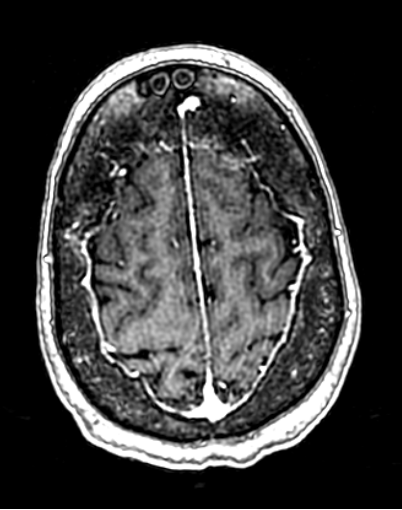
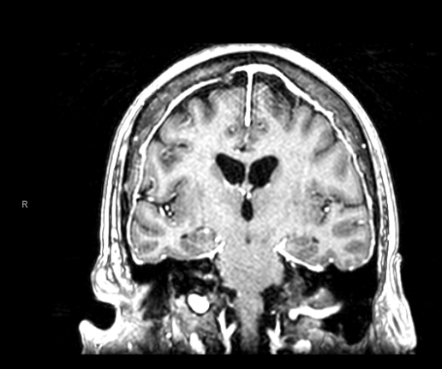
Case Presentation: A 49-year-old woman with a history of alcohol use disorder, hypertension, asthma, obesity, and prior lacunar stroke presented to a different hospital with seizure-like activity, encephalopathy, and right gaze deviation. Additional collateral history noted a year of progressive cognitive, bladder, and ambulatory dysfunction, resulting in wheelchair dependence.On admission, she was diagnosed with urosepsis from ESBL-producing Klebsiella pneumoniae, which was managed appropriately with IV antibiotics. However, she remained persistently encephalopathic. MRI of the neuraxis showed diffuse nodular leptomeningeal enhancement involving the brain and spinal cord. Lumbar puncture ruled out acute infectious meningitis and was negative for malignant cells but was notable for low glucose, elevated protein and elevated angiotensin-converting enzyme (ACE) levels in the CSF. No hilar lymphadenopathy or pulmonary infiltrates were noted on chest imaging. Empiric treatment for neurosarcoidosis involving intravenous immunoglobulins and high-dose glucocorticoids was started, resulting in rapid improvement in her encephalopathy. She was also noted to have central diabetes insipidus (CDI), characterized by high urine output (up to 9 L/day) and a positive water deprivation test. Leptomeningeal biopsy was negative for granulomas that characterize sarcoidosis, which was likely due to the recent receipt of high-dose steroids. Repeat CNS MRI showed resolution of leptomeningeal nodular enhancement but persistent cauda equina enhancement. She was discharged to a rehab facility on a prednisone taper, desmopressin, and infliximab.
Discussion: Our case describes a rare instance of presumed neurosarcoidosis presenting with diffuse leptomeningeal enhancement and CDI as its initial manifestation. CNS involvement in sarcoidosis is rare, affecting 5-15% of all patients with the disease. The subset of these cases involving the hypothalamus-posterior pituitary axis causing CDI is exceedingly rare, and its description is restricted to a few case reports.When evaluating a patient with neurological deficits and leptomeningeal enhancement on CNS imaging, it is important to consider infectious, inflammatory, and neoplastic etiologies. After infectious meningitis and cancer have been ruled out, it is vital to pursue a leptomeningeal biopsy early in the course of the illness if the diagnosis remains uncertain. Dramatic clinicopathological response to systemic steroids points strongly towards an inflammatory process. A thorough rheumatological evaluation should be undertaken to rule out common inflammatory diseases causing CNS involvement (e.g. RA, SLE, and vasculitides). CSF abnormalities in neurosarcoidosis are most pronounced in patients with diffuse leptomeningeal enhancement on MRI suggesting active disease. Improvement in CSF abnormalities may be a valuable tool for monitoring disease activity during therapy. Steroids combined with immunosuppressive drugs significantly improve response rates compared to steroids alone (69% vs. 35%). Radiation therapy to the CNS is an option for cases refractory to immunosuppression.
Conclusions: We describe a rare presentation of neurosarcoidosis – diffuse steroid-responsive leptomeningeal involvement and central diabetes insipidus. Our case highlights the importance of the role of hospitalists in expediently diagnosing inflammatory CNS conditions and pursuing neurosurgical consultation for meningeal biopsy if indicated.