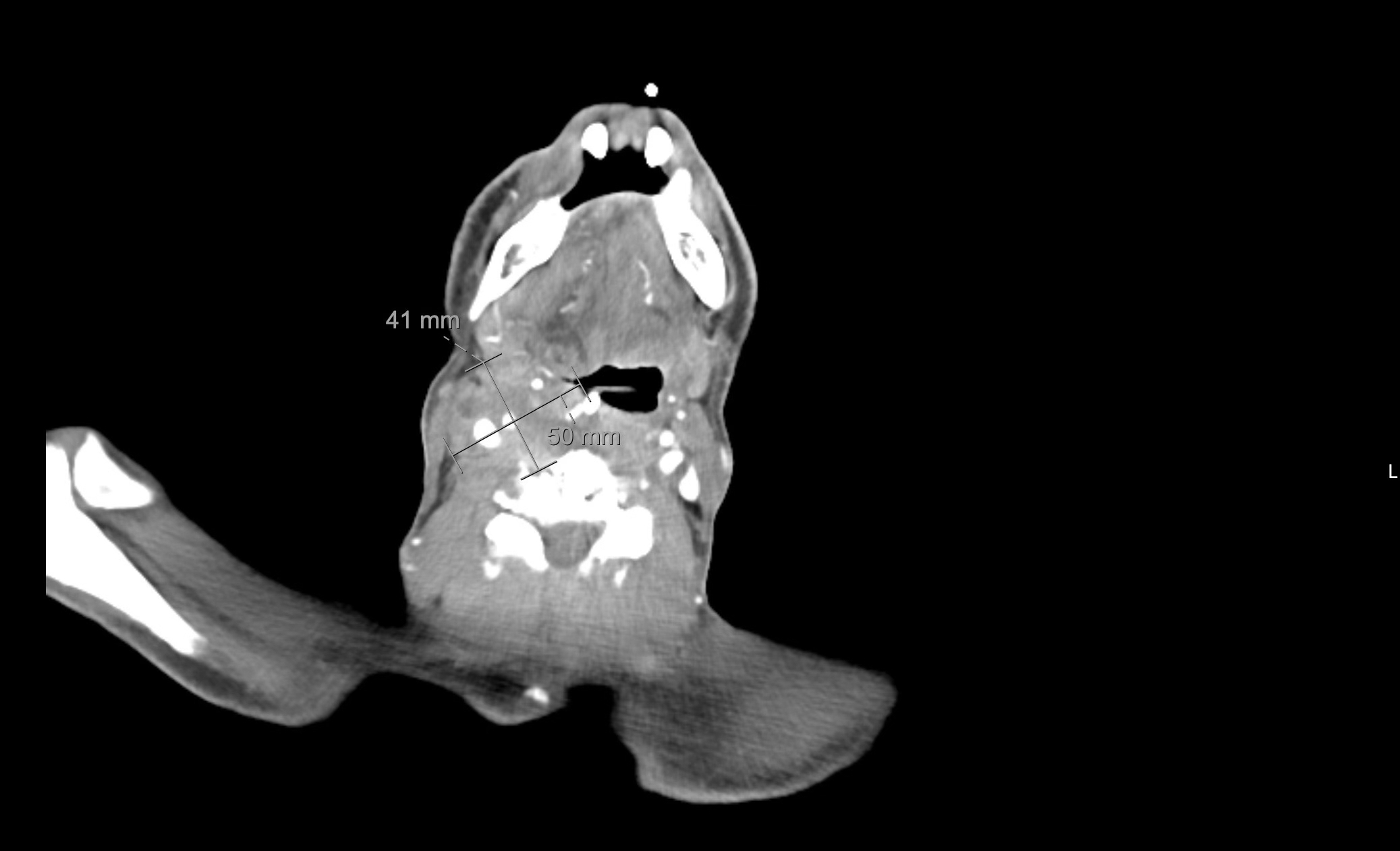
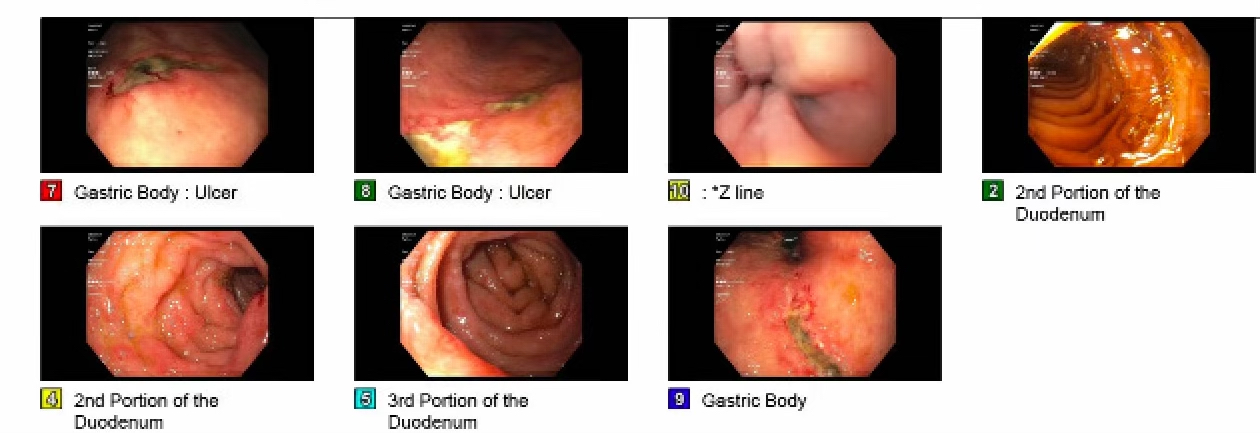
Case Presentation: 65-year-old man with a history of end stage renal disease on hemodialysis, hypertension, cervical spine stenosis status post surgical decompression presented with melena, a decreased appetite, dysphagia for solids and liquids, and a ninety-pound weight loss over the prior six months. He was admitted with acute hypoxic respiratory failure and stridor requiring endotracheal intubation. On exam, the patient was afebrile (temperature 36.6 C), heart rate 85, blood pressure 194/98, respiratory rate was 28, and O2 saturation was 82% on room air. He was ill-appearing, cachectic, had bitemporal wasting, was using accessory muscles and had stridor and a palpable right cervical neck mass. The remainder of the exam was normal. A CT of the chest, abdomen, and pelvis did not show any evidence of malignancy but a CT of the neck showed a large, multilobulated, heterogeneously enhancing mass (3.4 x 5 x 4.3 cm) of the right neck that was suspicious for a neoplasm versus necrotic lymphadenopathy with leftward deviation of the larynx and trachea. A core needle biopsy of the cervical soft tissue mass of right neck demonstrated adenocarcinoma infiltrating skeletal muscle. The neoplastic cells were positive for Cytokeratin 7 (CK7), Cytokeratin 20 (CK20), Caudal type homeobox 2 (CDX2), Focal GATA binding protein 3 (GATA3) and negative for Thyroid transcription factor 1 (TTF1), Paired box gene 8(PAX-8), Thyroglobulin and NK3 Homeobox 1 (NKX3-1); an immunohistochemical profile most suggestive of an upper gastrointestinal tract origin, and less likely pancreaticobiliary. A direct laryngoscopy and bronchoscopy showed no evidence of masses or lesions suggestive of a malignancy. An esophagogastroduodenoscopy (EGD) showed three gastric ulcers but no masses or lesions concerning for a malignancy. Biopsies of the gastric ulcers showed gastric/oxyntic mucosa with focal mild active inflammation, patchy intestinal metaplasia and regenerative change and random gastric and duodenal biopsies only showed chronic inflammatory and reactive changes but neither showed evidence of a malignancy. Immunostains for AE1/AE3 (pan-cytokeratin monoclonal antibody) and D2-40 (monoclonal antibody that binds to podoplanin) from the gastric and duodenal samples also ruled out the existence of occult tumor cells . An immunostain for H. pylori was negative. His condition progressively deteriorated and he was eventually transitioned to comfort care and he passed away.
Discussion: Cervical lymph nodes are a common site of metastases from primary head and neck malignancies and lymphomas but lymphatic spread of upper gastrointestinal (GI) malignancies more commonly involve the left supraclavicular lymph node (also known as Virchow’s node). While there are a few isolated cases in the literature that describe primary upper GI adenocarcinomas with metastatic spread to the cervical lymph nodes, there are no cases described in the literature of a primary upper gastrointestinal malignancy presenting as a solitary cervical lymph node mass without any malignancy identified in the GI tract.
Conclusions: This vignette is the first known case of a primary upper gastrointestinal malignancy presenting as a solitary cervical lymph node mass without any malignancy identified in the GI tract. Consequently, although rare, upper GI adenocarcinoma should be considered as part of the differential diagnosis of hospitalized patients who present with a cervical neck mass.