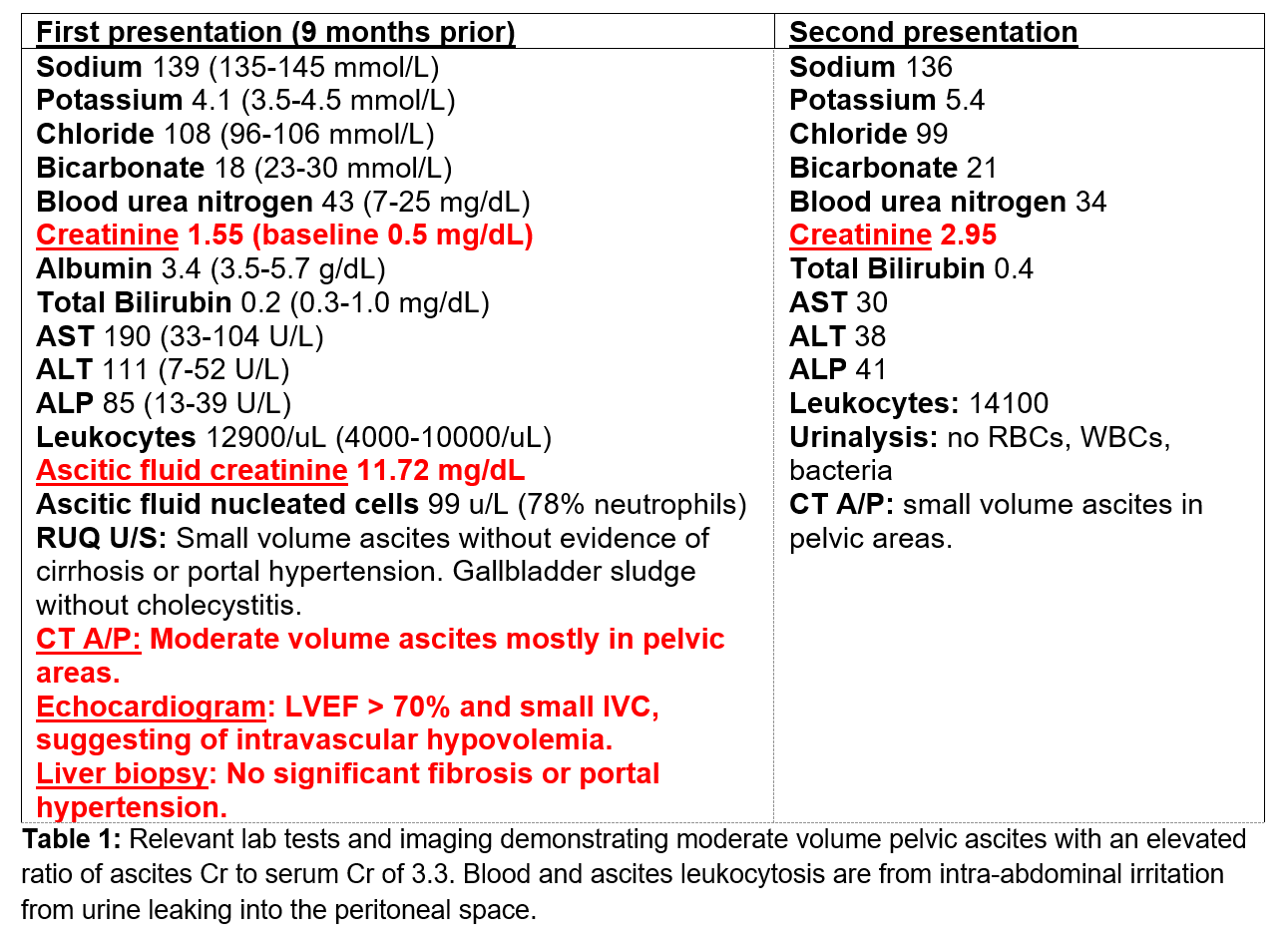
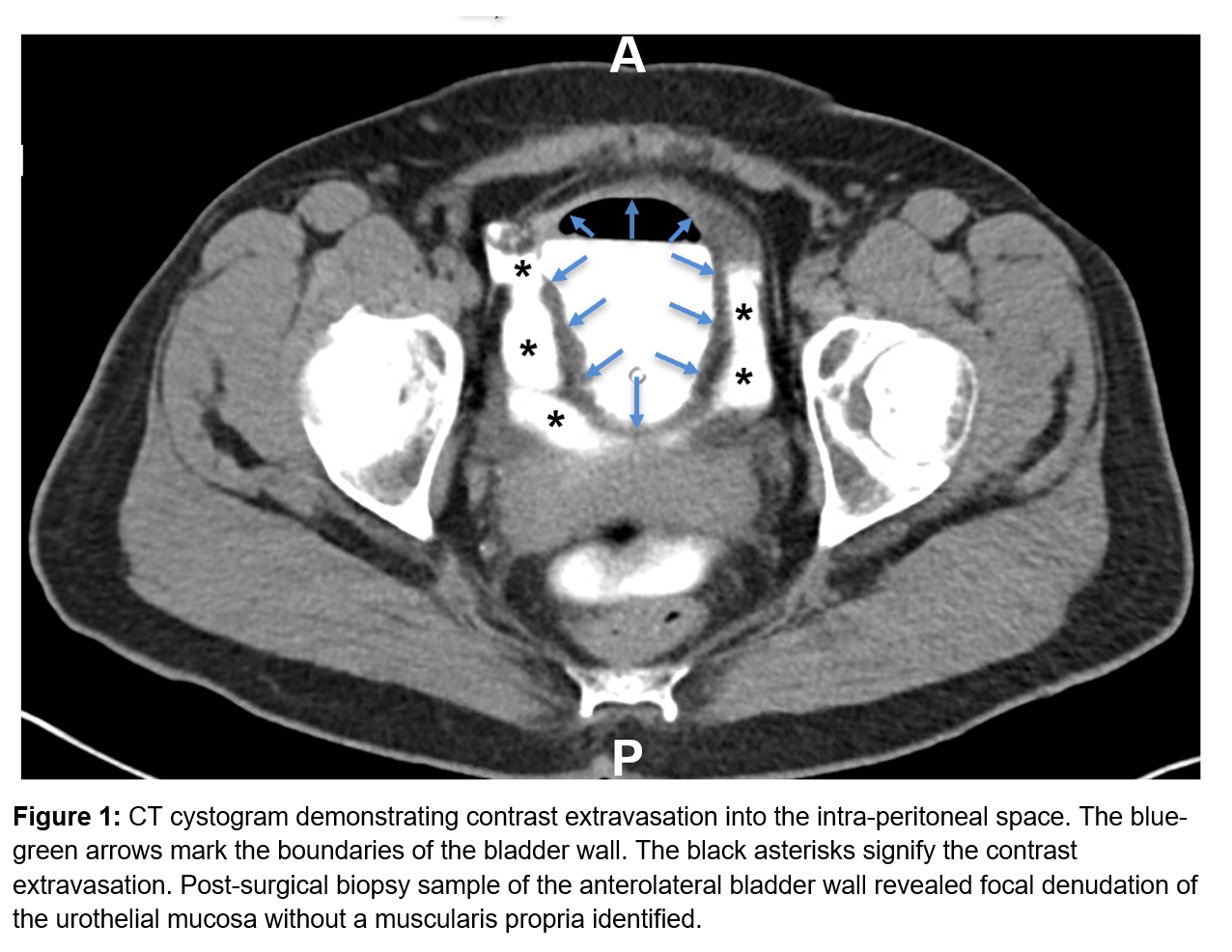
Case Presentation: We describe a case of new-onset unknown ascites due to atraumatic bladder rupture. A 56 year-old female with past medical history of functional urinary retention (prolonged urine holding due to phobia of public restrooms) and remote surgical history of TAH/BSO and C-section presented with recurrent ascites of unknown etiology. She initially presented to an outside hospital with ascites, which rapidly re-accumulated after paracentesis, as well as oliguria. She was transferred to our hospital for further evaluation. On initial admission, she had obvious abdominal distension without stigmata of chronic liver disease. Laboratory data revealed a BUN of 43, Cr 1.5 (Table 1). Abd U/S and CT A/P showed ascites without features of cirrhosis or portal hypertension (pHTN). SAAG was calculated to be 1.9 consistent with pHTN related ascites. There was no evidence for cirrhosis, Budd Chiari, portal vein thrombosis or right heart failure. Liver biopsy and echocardiogram were unremarkable. Further evaluation revealed an ascites Cr of 11.7 with a serum Cr of 3.5. Cr diffuses between plasma and the peritoneal space, therefore ascites and serum Cr should be the same. An ascites/serum Cr > 1 (patient’s 3.3) confirmed a urinary leak into the peritoneum. After urinary ascites was diagnosed, a foley was placed to divert urine and allow healing of a presumed micro-bladder perforation. After the foley was placed the serum Cr rapidly decreased from 3.5 to 0.5 in 48 hours because urine no longer leaked into the peritoneal space. A urogram and cystogram did not reveal a urinary leak. It was assumed the leak was too small to detect. She was discharged with a Foley for therapeutic bladder urinary diversion. The foley was removed 3 weeks later after urology follow-up. The patient did not have recurrence of symptoms until 9 months later when she presented with abdominal distention. CT A/P showed ascites too small for drainage. Given her history of presumed bladder wall rupture, a cystogram was repeated, revealing a bladder wall defect with intraperitoneal contrast (Figure 1). Urology performed an exploratory laparotomy and repaired a 2mm right anterolateral bladder perforation and placed a JP drain. Drain Cr was the same as serum Cr indicating no urinary leak. Pathology from the bladder dome biopsy revealed denuded mucosa without muscularis propria. She was discharged with a foley. Repeat cystogram upon follow-up two weeks later showed no leak, and the foley was removed.
Discussion: Urinary ascites should be considered in the evaluation of unexplained pHTN related ascites. As a mimic of pHTN related ascites, urinary ascites typically has a SAAG equal or > 1.1. If suspected, ascites Cr should be obtained with a paracentesis. An ascites:serum Cr ratio > 1 is diagnostic of urinary ascites due to urine leaking into the peritoneal space. Reabsorption of peritoneal Cr into the blood via diffusion increases serum Cr causing pseudo-renal failure. Although rare, long-standing episodic urinary retention can weaken the bladder dome, causing mucosal atrophy predisposing to rupture, as seen in this patient.After diagnosis, a foley should be placed for therapeutic urinary diversion, and a urogram and cystogram performed to investigate for urologic tract defects. Urology should be consulted for immediate surgical repair.
Conclusions: Urinary ascites should be considered in a patient with unexplained apparent pHTN related ascites. An additional clue to the presence of urinary ascites is the very rapid improvement in serum creatinine after foley placement.