Background: Rural areas are disproportionately affected by physician shortages, and small rural hospitals in particular struggle to staff acute medicine services 24/7. Telehospitalist models are emerging as an alternative to provide inpatient medicine services in rural settings. In a 2018 needs assessment of rural Veterans Health Administration (VHA) hospitals, 60% percent reported being short on hospitalist physician staff for the current year, 96% reported vacancies resulting in staffing difficulties in the last three years, and >70% were interested in partnering on a telehospitalist program.
Purpose: The goal of this quality improvement project was to develop, pilot, and evaluate the first telehospitalist service in VHA to provide staffing to a small rural hospital
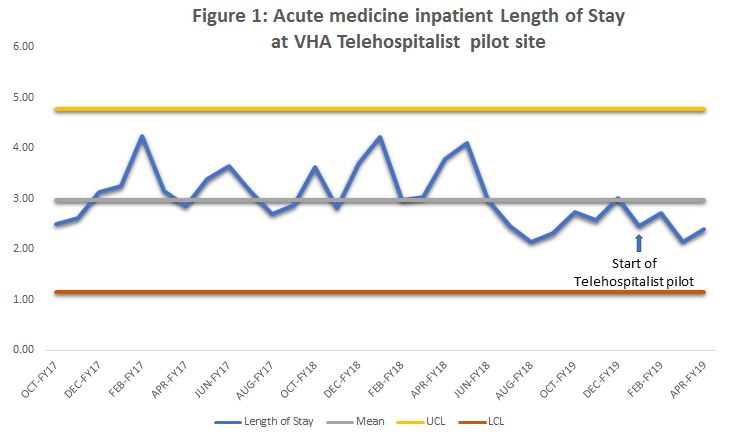
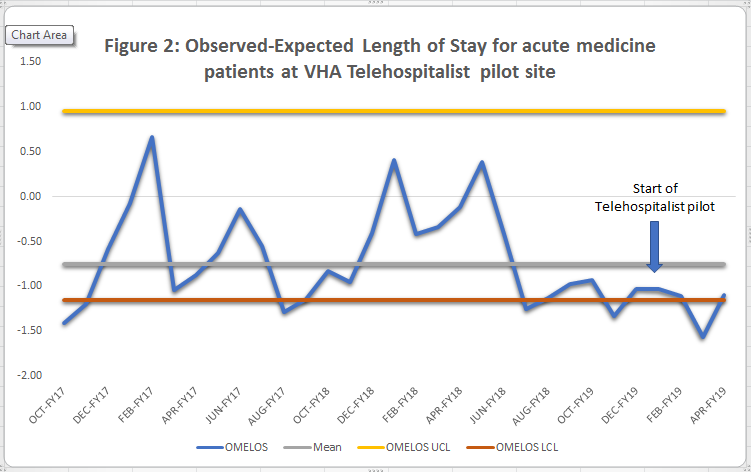
Description: After completion of a national needs assessment, a hospital was selected for a 4 month pilot phase (January – April, 2019) followed by consolidation phases of the service (July 2019 – present). Here we present the results of the pilot phase. Experienced telehospitalists based at a tertiary VHA hospital provided staffing for a 10-bed inpatient unit at a rural VHA hospital, Monday – Friday, 8am- 4:30pm. The telehospitalist service was staffed at the rural hospital with a nurse practitioner. Statistical process control charts were used to observe special cause variation over time. Process metrics included number of patient encounters, average patient encounters per day, and average workload. During the pilot phase, the telehospitalists participated in 530 encounters with an average of 6.2 per day, and average workload of 7.1 hours. Balancing metrics of 30-day readmission and mortality saw no significant changes during the pilot phase. Outcome metrics included length of stay (LOS), observed minus expected LOS (OMELOS), and patient and provider satisfaction. LOS and OMELOS remained at or below the baseline mean during the pilot phase. (Figure 1 and Figure 2) Initial feedback from patients and staff at the pilot site was mostly positive. Using staff surveys (n=15), patient feedback cards (n=6), and qualitative interviews (n=14), our summative evaluation identified that the high quality of care, teamwork, interpersonal communication, improved documentation, and responsiveness of the service contributed to the success of the program. Half (54%) of staff survey respondents reported a good or excellent overall experience with the telehospitalist service. Challenges included technology and communication issues; higher than anticipated workload and documentation requirements; differences in local practices; clinical concerns regarding delayed/missing orders; and difficulty contacting the telehospitalist.
Conclusions: A telehospitalist model is a feasible option to address hospitalist shortages in rural VA hospitals with no deleterious effects on quality or efficiency. Detailed explanation of services, clarification of expectations, and telehospitalist training on culture and resources at the receiving site were key factors for successful deployment. Ongoing channels to provide timely bidirectional feedback are necessary to ensure continuous program improvement and sustainability in a dynamic environment.