Background: Medical errors in hospitals are a significant threat to patient safety and often result from poor communication or poorly-activated interprofessional teams. Despite a recent focus on interprofessional education (IPE) in pre-clinical years and simulation settings, formal curricula for teaching medical trainees interprofessional communication and teamwork skills in clinical settings are lacking.
Purpose: To create an inpatient curriculum for medical residents that improves Interprofessional communication and teamwork behaviors and attitudes.
Description: I created a feedback curriculum based on the TeamStepps framework for attending hospitalist physicians on inpatient medical wards at a community teaching hospital. Medical and transitional residents rotate in 4 week blocks on team-focused inpatient units called Accountable Care Units (ACU). Teaching attendings were trained to give daily feedback to medical residents during interdisciplinary bedside rounds on: 1) communication, 2) leadership, 3) mutual support, and 4) situation monitoring. The curriculum began in July 2017. To evaluate the impact of the curriculum, we observed resident teamwork behaviors on interdisciplinary bedside rounds at the beginning and at the end of the rotation and surveyed residents on their teamwork attitudes. We conducted focus groups with the residents at the end of their rotation about the value of IPE.
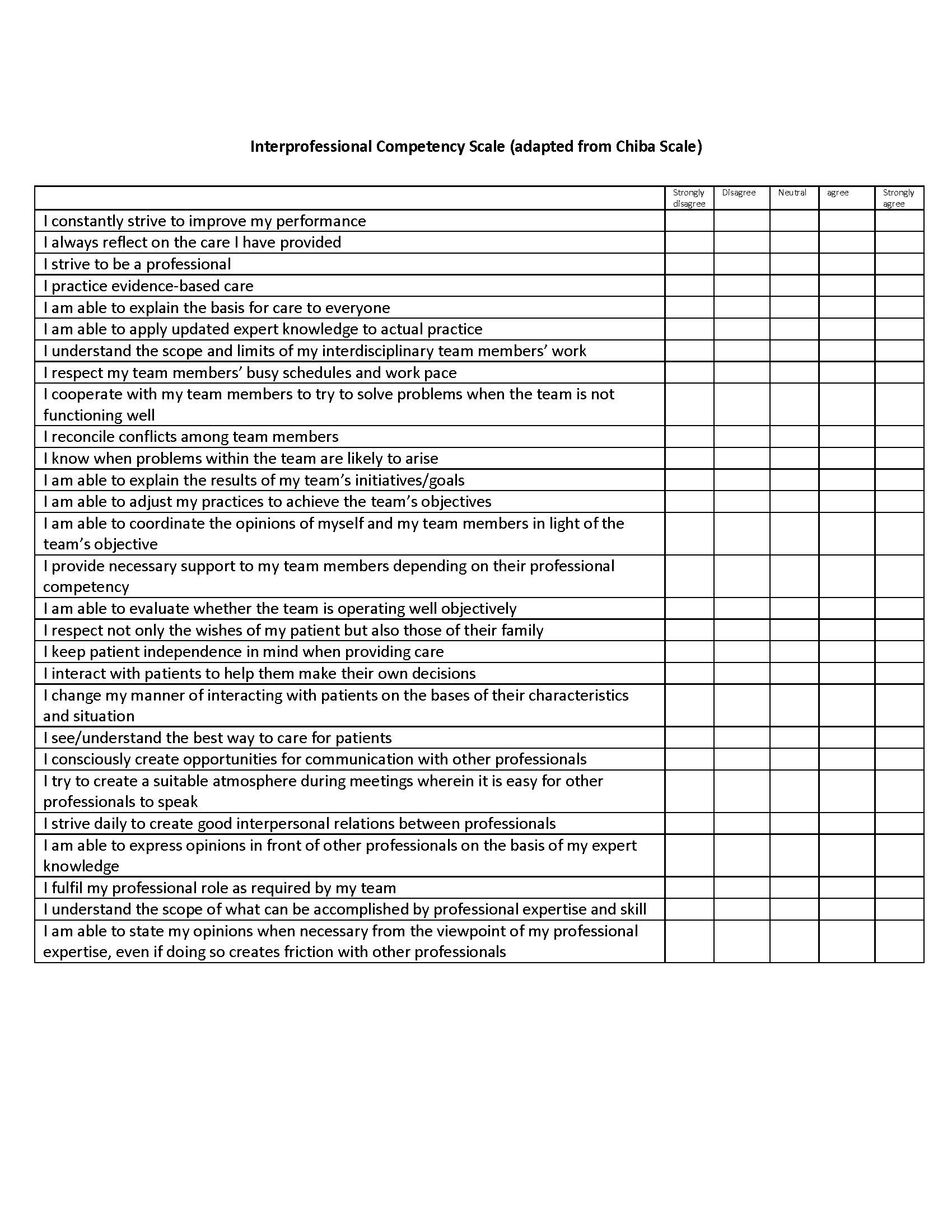
Conclusions: To date, forty-two residents have participated in the feedback curriculum. Preliminary data show that both interns and residents felt equally highly proficient in teamwork attitudes and skills prior to beginning the curriculum. Typically, all residents either agreed or strongly agreed that they regularly do the 28 highly advanced teamwork behaviors listed on the adapted Chiba interprofessional competency scale. While the senior residents experienced no change in their teamwork skills at the conclusion of the curriculum, first-year residents consistently reported that they improved these skills by the end of the rotation. Residents who led interprofessional bedside rounds consistently performed more team-centered behaviors at the end of the feedback curriculum as compared to the beginning of the curriculum. Through focus groups, we have identified interesting trainee beliefs about IPE: 1) medical knowledge proficiency must precede learning about how to work in teams, and 2) teamwork behaviors are learned at an early age and remain static throughout life. These beliefs may help inform future IPE curricular design. Data collection is ongoing but thus far, results show that residents perceive that they have a high level of proficiency in interprofessional teamwork and communication skills; interns may be more open to feedback about teamwork behaviors than senior residents. The daily feedback curriculum consistently improves resident communication and teamwork behaviors on interprofessional bedside rounds.