Background: Cognitive load (CL) is increasing in healthcare leading to provider frustration and poor performance. Human factors design principles like cognitive load theory (CLT) may mitigate the negative impacts of CL. This study examined the impact of a post-hospital dashboard (PHD) designed using CLT on provider performance and perceptions of workload in the post-hospitalization visit.
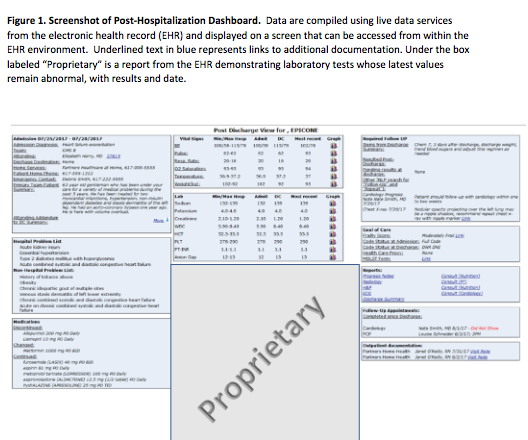
Methods: This was an unblinded, randomized controlled non-clinical trial using asimulated post-hospital discharge visit and a standardized virtual patient in the electronic health record (HER). Participants (41 of 140 invited) were volunteer medicine residents and attending PCPs in an academic medical center. Participants were randomized to usual care (data in the EHR) or usual care plus a post-hospitalization dashboard (PHD) (figure), which organized relevant information in a manner designed to decrease CL. The primary outcome was number of appropriate actions taken (max: 8) based on participant documentation in the record. Secondary outcomes included identification and documentation of each safety risk, time to complete the visit, and CL. The NASA task load index (NASA-TLX) measured CL and reported it as an overall score from 0-100 based on a weighted average of six subscales of demand: mental, physical, temporal, performance, effort, and frustration. Unadjusted outcomes between arms were compared using Wilcoxon rank sum tests. We calculated unadjusted differences in medians and inverted the Wilcoxon rank sum test to generate 95% confidence intervals.
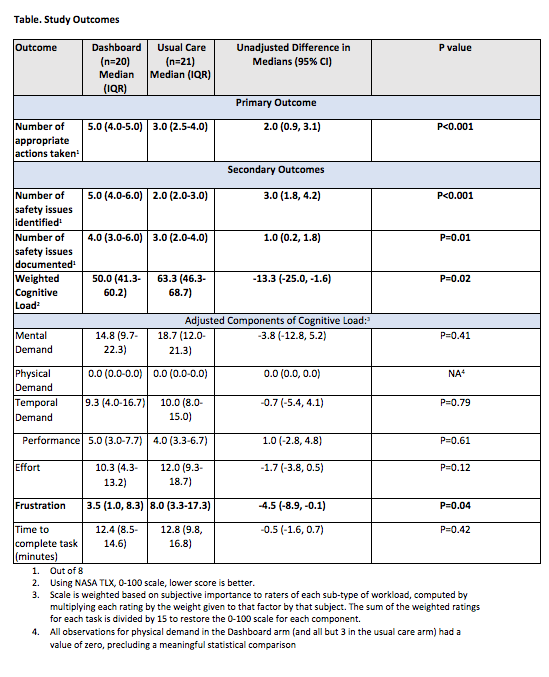
Results: The intervention arm had 20 participants and 21 were in the usual care arm. Possible confounders (sex, resident status, and post-graduate year) were similar in the two arms. Participants using the PHD documented a median of 5.0 (IQR 4.0-5.0) of 8 appropriate actions taken vs. 3.0 (IQR 2.5-4.0) of 8 in the usual care arm (difference in medians 2.0, 95% CI 0.9 – 3.1, P<.001). Similar differences were seen with the number of safety issues identified and documented. Median weighted CL was 50 with the PHD versus 63 with usual care, p=0.02. The median adjusted frustration subscale was 3.5 (PHD) vs. 8.0 (usual care), p=0.04. There were no significant differences in time to complete the visit (Table).
Conclusions: Tools informed by CLT may improve provider performance by decreasing the likelihood that critical data is missed and decreasing frustration. This hypothesis needs to be further studied in live patient interactions.