Background: In hospital-based medicine, maintaining an open line of communication between inpatient teams and community pediatricians serves as an essential component of providing comprehensive patient care and ensuring continuity at time of discharge. At St. Louis Children’s Hospital, inpatient resident teams are responsible for providing timely communication with community pediatricians regarding major patient events. Despite being a known responsibility of resident physicians, there has historically been no standardized process to incorporate community pediatrician updates into daily resident workflow. The absence of a standardized process has led to frequent gaps in communication that can poorly affect hospital relationships with community pediatricians and hinder the continuity of patient care.
Purpose: To improve communication between general medicine inpatient resident teams and community pediatricians (PMDs) through the development and implementation of a standardized workflow and documentation process.
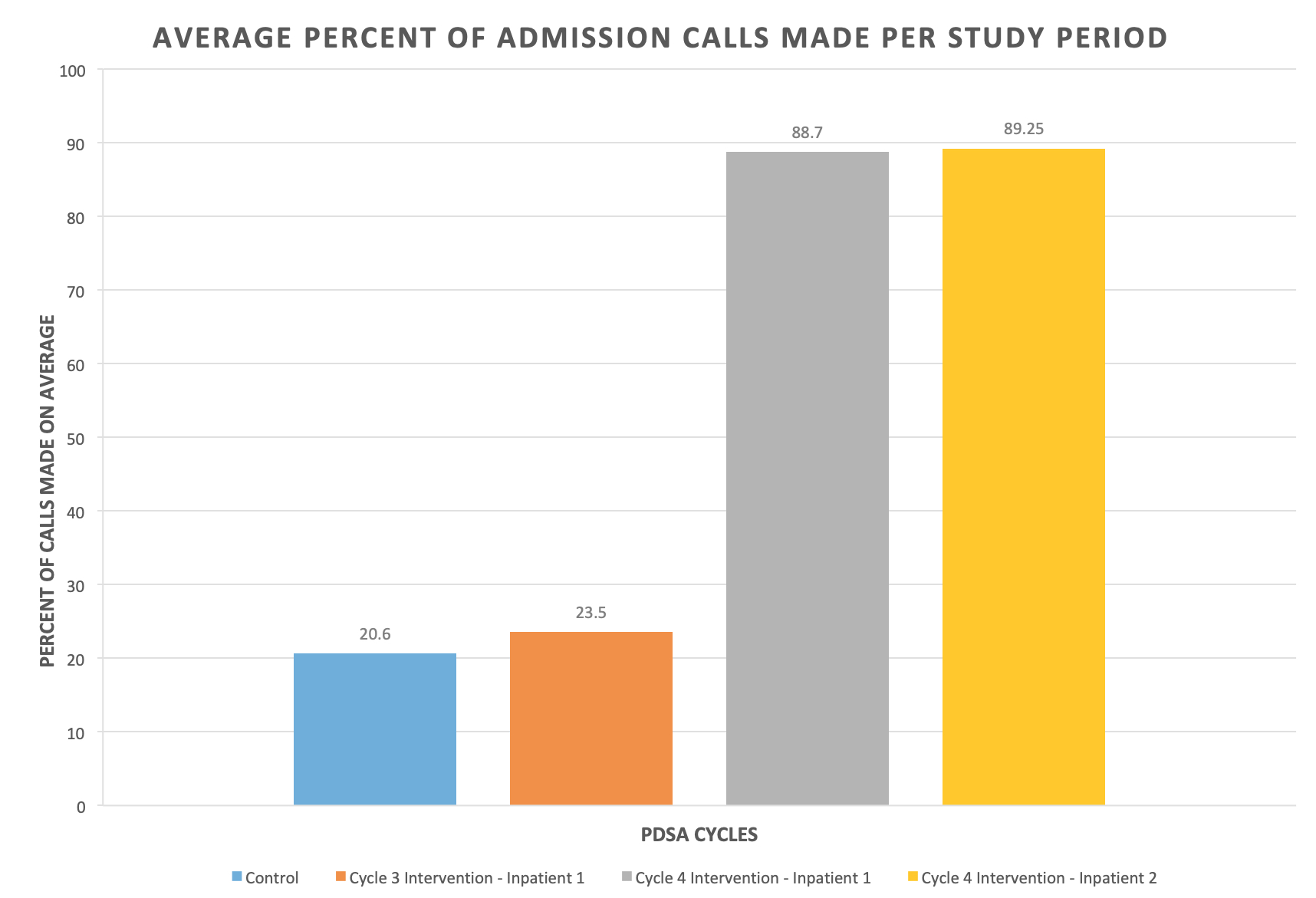
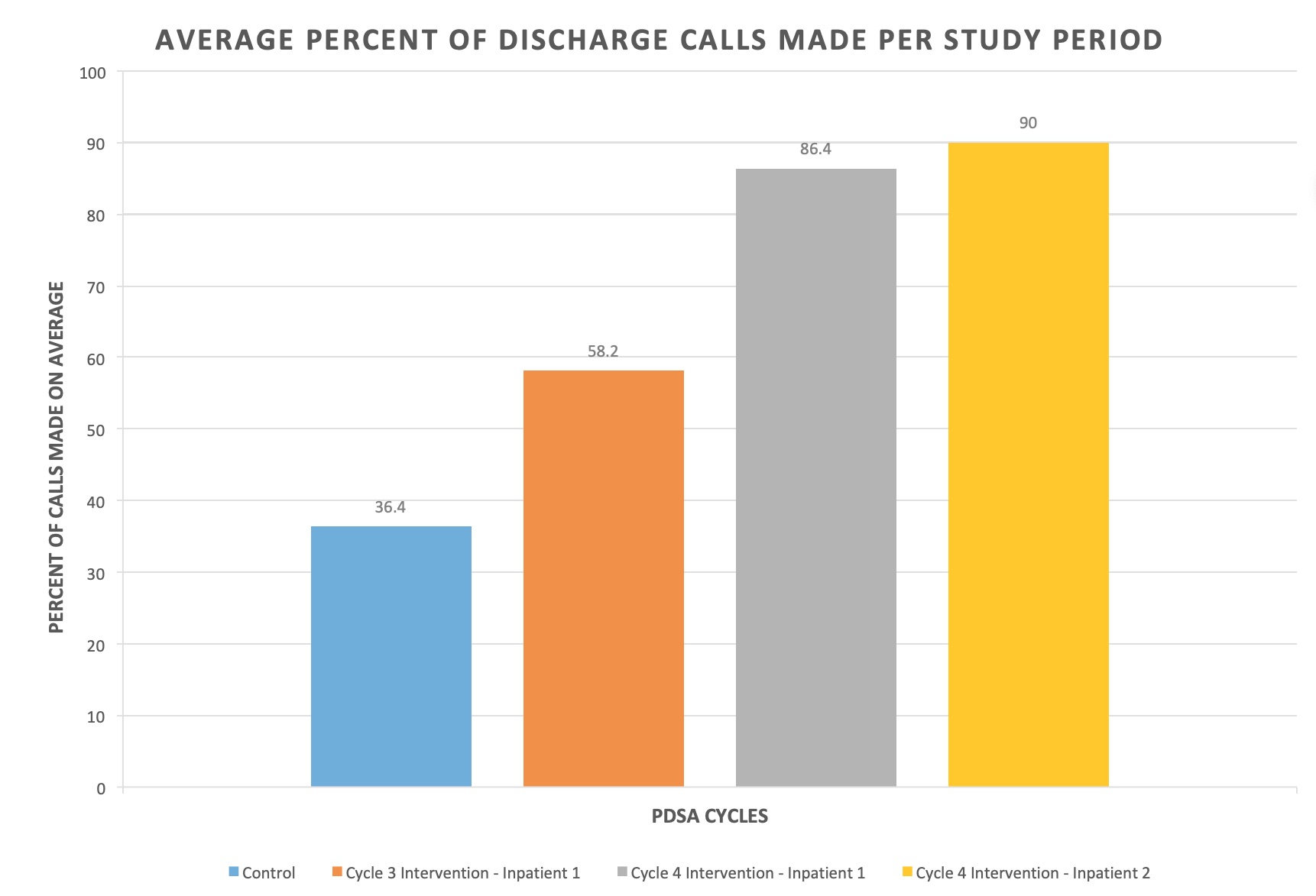
Description: An initial residency-wide survey was administered to identify barriers to providing timely pediatrician updates. Based on the results, a series of staged interventions were implemented through four Plan-Do-Study-Act (PDSA) cycles over a one year time period. PDSA Cycle 1 focused on clarifying communication expectations through the distribution of a “PMD Communication Guidelines” document to inpatient resident teams, as well as a script of a sample update call for reference. For Cycle 2, the senior resident was encouraged to discuss PMD updates at the conclusion of each patient presentation during morning rounds and assign a specific team member to make the call, if necessary. Modest subjective improvement was observed with these interventions over a 2-week period; however, logistical challenges with data collection limited interpretation. Cycle 3 repeated interventions from Cycle 2 over a 2-week period, while also incorporating “PMD Communication” into the nursing rounding checklist, with the hope of engaging interdisciplinary team members. Improvement from a baseline average of 20.4% of admission and 36.4% of discharge calls to 23.5% of admission and 58.2% of discharge calls was identified (Figures 1 and 2). Cycle 4 expanded on the interventions from Cycles 2 and 3 by including two general medicine inpatient floors, again over a 2-week period. The “PMD Communication Guidelines” document was updated and re-distributed, and documentation of PMD updates was encouraged by creating a section within the resident handoff to reflect the last date a PMD call was made and the next planned update. With these interventions, the average percent of admission calls improved to 88.7% and 89.25% on the two general medicine inpatient floors trialed, and discharge call rates improved to 86.4% and 90% (Figures 1 and 2).
Conclusions: The development of a standardized workflow and documentation process improves the rates of timely communication between inpatient general medicine resident teams and community pediatricians.