Background: Statistics show at least 5.7 million Americans have a diagnosis of heart failure (HF), and they account for >1 million admissions every year in the United States. Prolonged length of stay (LOS) often leads to higher mortality and increased healthcare costs. At our urban tertiary academic medical center, we have incorporated a Microsoft Teams cloud-based information technology tool known has “myNora” and developed a heart failure (HF) information card. This card provides daily standing weights, positive or negative changes to weight, fluid intake and urine output, to help guide IV diuretic therapy. We aimed to improve patient outcomes and length of stay by utilizing this HF tool.
Purpose: The goal of this project is to see if assessing diuretic therapy during interdisciplinary rounds (IDRs) and adjusting medications early in the day affects length of stay for heart failure admissions.
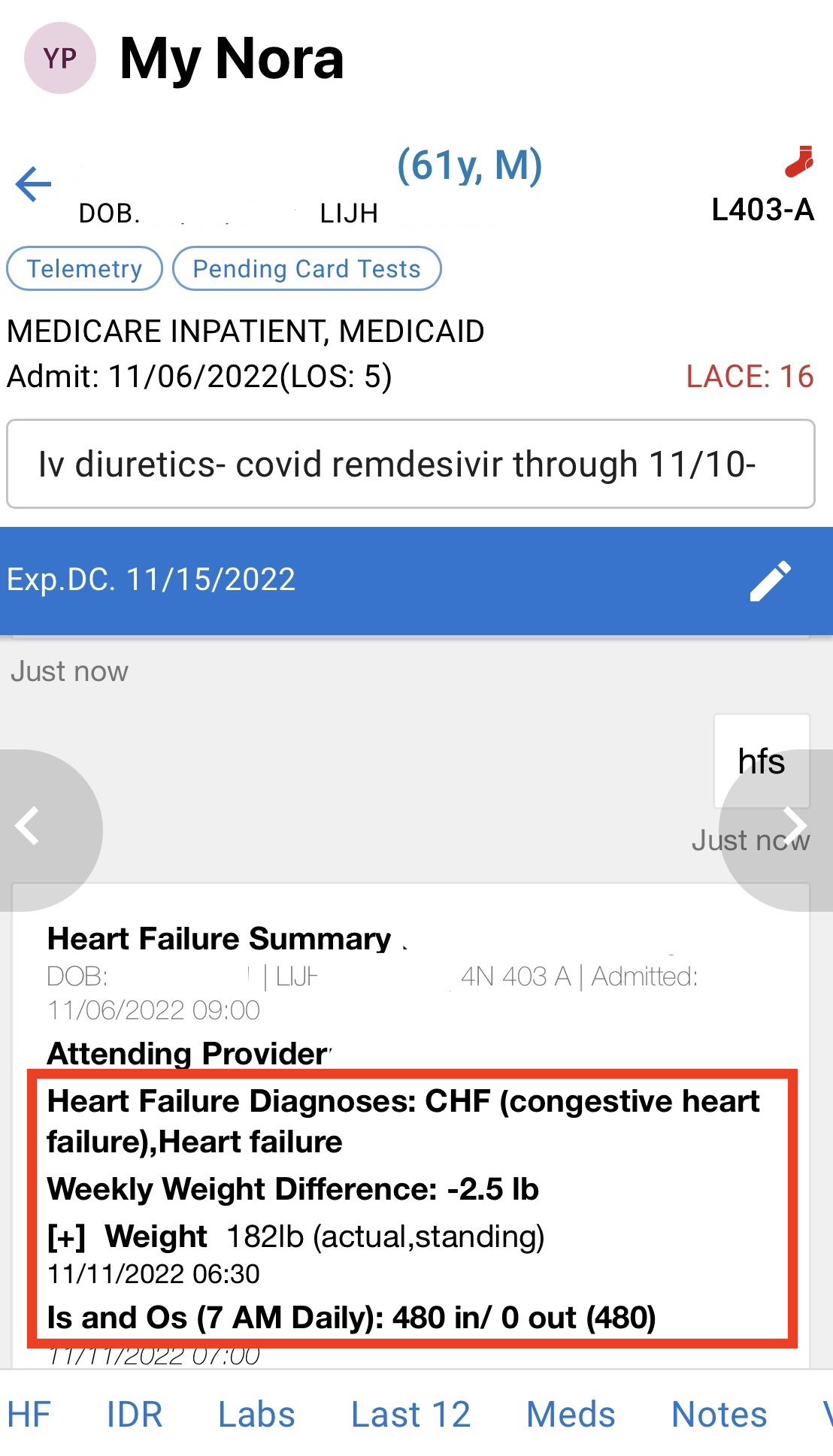
Description: The HF card was created in our MS Teams app which is used to guide morning IDRs. It has been implemented at our center on our cardiac telemetry unit, 5N, since April 2022. This initiative is hospitalist and nursing driven. The hospitalist identifies patients on the unit who have acute heart failure or heart failure exacerbation as the admitting diagnosis. The nursing staff then obtains daily standing weights and enters them into the EMR. During IDRs, we refer to the daily weight change listed in the card for all HF patients and make real time changes to medications, typically diuretic agents. These changes include dosing, frequency and adjustments to alternate therapies if the original diuretic is not adequately working. Preliminary data was pulled for patients on 5N for two time periods, April to June in 2021 and in 2022. Strictly comparing LOS, there was a modest decrease in LOS, from 8.71 to 7.58 in the month of April and from 7.47 to 5.29 in the month of June. Some limitations include, bed weights as opposed to standing daily weights and inaccurate inputs and outputs if the patient has brought beverages from outside the hospital. Our data collection period was truncated due to the conversion of 5N into a COVID unit.
Conclusions: Using the information provided by the HF card has led to efficient care for our patients and decreased length of stay as seen by our preliminary results. Next steps would be to gather data on heart failure readmission rates since implementation of our project. In addition, despite the well-established role of GDMT for HF management, many hospitalized patients are discharged on suboptimal medications. With the assistance of the MyNora HF card, we aim to closely track current medications a patient is on and ensure they are discharged on appropriate GDMT (beta blockers, ACE/ARB/ARNI, etc).