Background: Communication failures amongst interdisciplinary internal medicine (IM) teams occur often in the inpatient setting, which can inhibit mutual understanding of care plans, increase the potential for medical error, and contribute to patient dissatisfaction. Efforts to enhance interdisciplinary collaborative teamwork within inpatient IM teams highlighted a critical need to address concerns related to communication.
Methods: We conducted a single-center participatory mixed methods study using both group level assessment (GLA) and concept mapping to examine current barriers and facilitators of effective communication. Both GLA and concept mapping follow structured processes designed to engage diverse groups of stakeholders in the inquiry process. Our recruited stakeholders were IM faculty, residents, nurses and ancillary staff, patients/families, and care managers who work or have experienced care on inpatient IM teams at an 800-bed tertiary academic hospital. Stakeholder-specific GLA sessions were conducted where participants first responded individually to open-ended prompts addressing interdisciplinary communication (e.g. Ideal methods of communication include). Following generation of individual responses, participants worked in small groups to synthesize the qualitative data and identify key ideas. Concept mapping was then used to sort these ideas using a web-based platform and then use multidimensional scaling and hierarchical cluster analysis to generate a concept map visually representing the data.
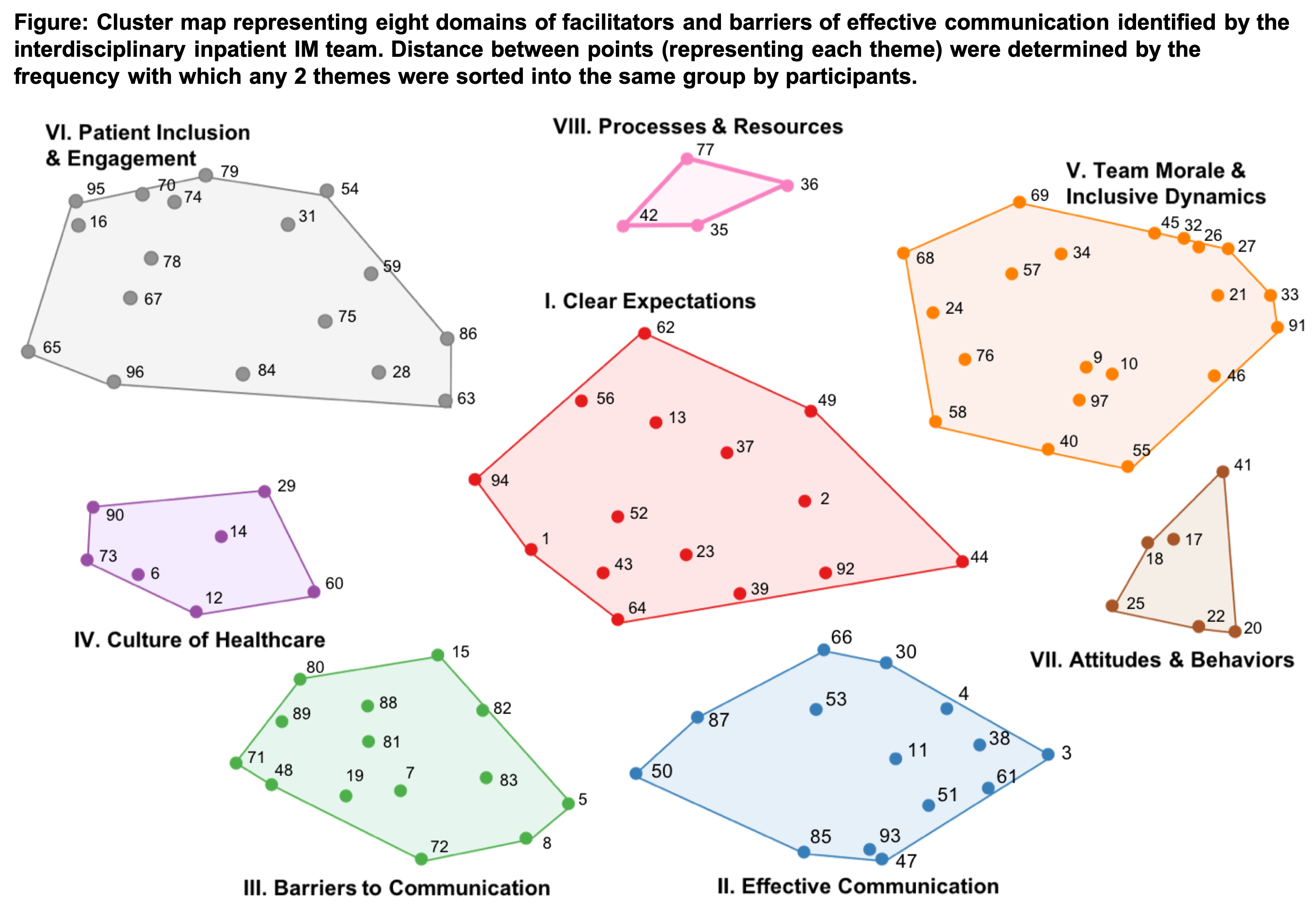
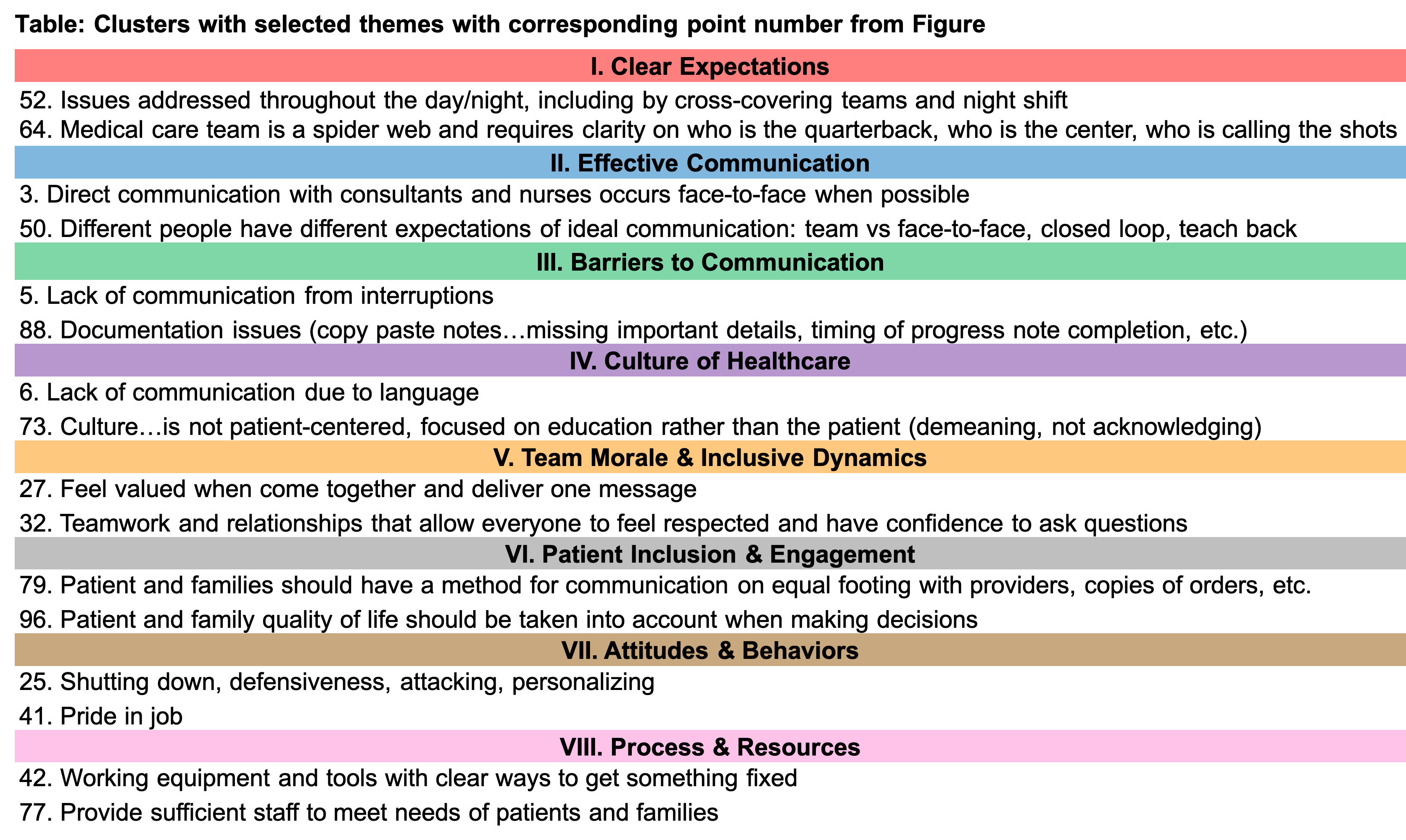
Results: We recruited 104 stakeholders (17 care managers, 16 nurses and ancillary staff, 22 IM faculty, 19 patients and families, 30 residents). GLA sessions revealed 97 unique ideas (Table with subset of ideas). After stakeholder sorting, subsequent analysis revealed an eight-cluster concept map (Figure) showing how the arrangement (i.e. location and distance between) of the 97 ideas, illustrated by points, have meaning. Each of the eight clusters represents ideas sorted together due to conceptual similarity. Clusters emphasized three key conceptual domains: patient inclusion and engagement (Clusters IV, VI), institutional expectations and role clarity (Clusters I, II, III, VIII), and team dynamics and behaviors (Clusters V, VII). Centrality of clear expectations and its subsequent prioritization by all stakeholder groups has now informed next steps for improvement work.
Conclusions: We demonstrated feasibility of using a structured participatory approach in the inpatient setting across stakeholder groups to identify facilitators and barriers of effective interdisciplinary communication within the inpatient IM teams. By interpreting the relationship between ideas and the perspectives of other team members, inpatient IM team stakeholders have identified clear expectations as a central and prioritized area to target interdisciplinary communication improvement efforts.