Background: New internal medicine interns are expected to be familiar with bedside procedures such as paracentesis. Medical students frequently have inadequate dedicated time to learn bedside procedures and are taught in a fragmented manner. As a result, new interns lack familiarity with these procedures. As such, we assessed whether a comprehensive module for paracentesis would improve fourth-year medical student comfort and competence compared to standard training.
Methods: We developed a novel comprehensive module in our Residency Essentials Course – Internal Medicine Track to teach paracentesis. The module covered ten key areas about paracentesis. Students enrolled in our track were included and stratified into two groups based on their future residency specialty. Students answered a pre-practice survey of 9 questions related to paracentesis indications, technique, complications, and lab interpretation. The first group (specialties Internal Medicine, Medicine-Pediatrics, Interventional Radiology, Physical Medicine and Rehabilitation) received standard instruction, which included an online procedural animation video from NEJM to review. The second group (specialties Emergency Medicine, Family Medicine, Anesthesia, Neurology) were provided the comprehensive module. Students from both groups were divided into groups of 2-3 and received thirty minutes of practice time with task trainers supervised by resident/faculty instructors. Both groups completed a post-practice multiple choice quiz and post-practice survey and were evaluated by faculty on their practical procedural competence. The scoring for the practical had 2 components: a numerical checklist score of 100 points and a pass/fail on mastery of the technique. Nine students were excluded from this study because they were unable to practice on task trainers.
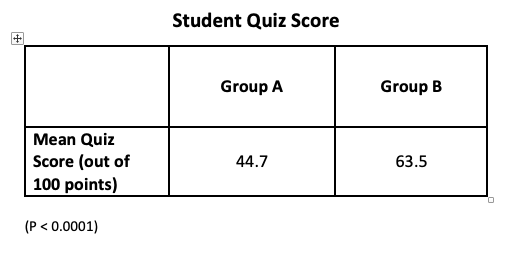
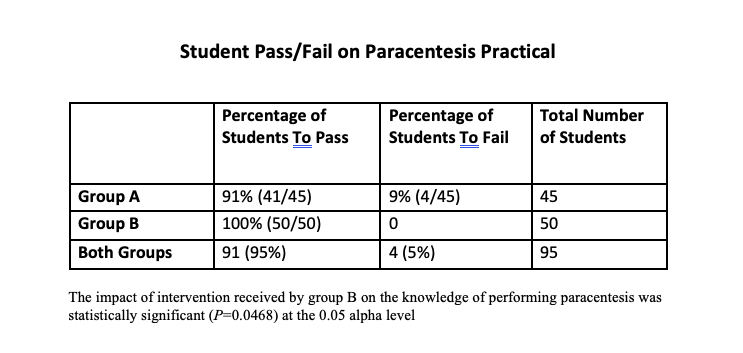
Results: 107 fourth-year medical students were included in the study. There was no significant difference in age or gender between the two groups. The median value for each pre-practice survey question varied between 3 or 4 on the Likert scale. There was no significant difference between the 2 groups suggesting a comparable baseline comfort value. The intervention arm had significantly higher quiz scores (mean score of 63.5 in B vs. 44.7 in A out of 100 points; P<0.0001) and practical competence pass rate (100% pass rate in B vs 91.1% in A; P=0.0468). The numeric checklist score was not statistically different amongst the 2 groups (mean score of 93.3 in B vs. 90.2 in A out of 100 points; P=0.1395). Both groups A and B responded as being more confident in the post-practice survey (83.78%) as compared to the pre-practice survey (62.50%; P=0.0302). Students in Group B felt more confident in recognizing labs to order for paracentesis (Odds Ratio=3.5; 95% confidence interval [CI], 1.0876-11.0503). There was no association between student confidence in post-practice survey and their quiz score or checklist score.
Conclusions: Our novel module was associated with better quiz scores and practical competence. Our study suggests that a comprehensive paracentesis module may improve student comfort and competence with procedures. This could help guide future curriculum development for procedural training. Future studies are needed to evaluate whether our framework would apply to other procedures or in other institutions.