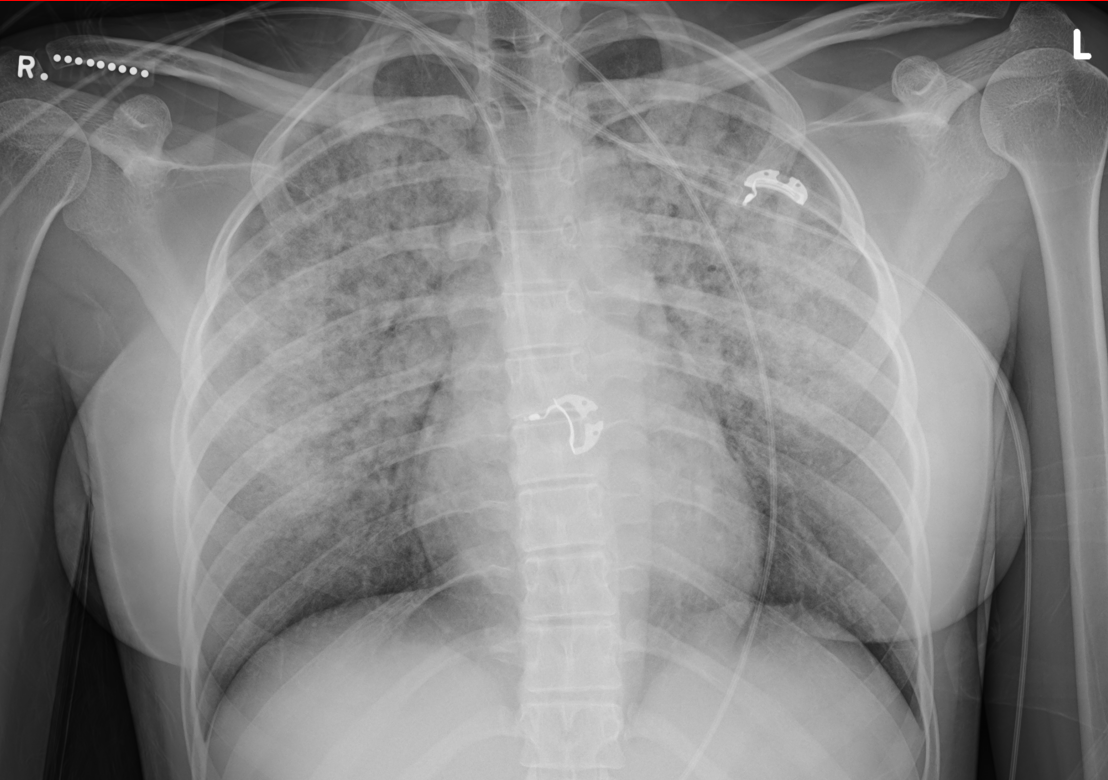
Case Presentation: An otherwise healthy 19 year old female was evaluated for acute dyspnea, hemoptysis, and throat pain after e-cigarette use with and without marijuana. She had taken oxycodone for throat pain and had received naloxone in the field for altered mentation. On arrival, she was afebrile, tachycardic, saturating 92% on 4L via nasal cannula. She became progressively more dyspneic, leading to intubation. Admission labs showed a lactic acidosis but otherwise normal cell counts, inflammatory markers and comprehensive chemistries. Urine drug screen was positive for cannabis. Chest x-ray showed bilateral infiltrates (Figure 1). She underwent bronchoscopy which revealed bloody secretions with progressively less hemorrhagic aliquots. Cell counts from bronchial washings showed scant cellularity and a comprehensive evaluation for bacterial, fungal and viral pathogens was negative. An autoimmune workup was similarly unrevealing. She was intermittently febrile and inflammatory markers rose (CRP 223mg/L). After a thorough negative workup, and given her refractory hypoxia in the background of known e-cigarette use, she was given methylprednisolone for electronic cigarette or vaping associated lung injury (EVALI). She was successfully extubated and on hospital day five the patient was discharged with supplemental oxygen and an oral prednisone taper. Three weeks after discharge there was complete radiographic resolution, but persistently reduced DLCO (72% predicted) on pulmonary function tests.
Discussion: EVALI is an emerging disease entity, recognized after a multistate epidemic in 2019 that persists despite federal, state, and industry attention. Originally studied as a tobacco cessation aid, e-cigarettes are no longer recommended by multiple academic societies. Steroids were administered in this case, but evidence supporting its use is limited to case series and expert opinion. As in this case, EVALI may cause pulmonary parenchymal damage demonstrated in some studies as spirometry abnormalities and most commonly reductions in carbon monoxide diffusion capacity. Steroid administration may be warranted to ameliorate this lung damage, until additional studies are published. Due to the addictive nature of vaping, these patients are risk for re-exposure, recurrent or worsening EVALI, and readmission. Hospitalists should address tobacco use disorder with nicotine replacement therapy, if appropriate, and emphasize the importance of e-cigarette abstinence after discharge with close outpatient follow-up.
Conclusions: EVALI may be diagnosed in patient with suggestive exposure after infectious and autoimmune etiologies are excluded. Although systemic steroid therapy may not be necessary for every case, hospitalists should consider steroid administration, unless otherwise contraindicated, given known pulmonary function abnormalities that persist after discharge.