Background:
Patients hospitalized for acute medical illness may be at increased risk for venous thromboembolism (VTE). Identifying those medical patients most at risk for VTE is of increasing importance and emphasized in recent guidelines. Several risk assessment models (RAMs) exist, but their ability to accurately determine VTE risk in medical patients is not clear. The Michigan Hospital Medicine Safety Consortium (HMS), a state‐based quality collaborative aimed at preventing adverse events in hospitalized medical patients, reviewed various RAMs in an effort to determine which model(s) has the most utility for medical patients. Additionally, the collaborative developed its own model based on data collected from hospitals throughout the state of Michigan.
Methods:
Using web‐based data entry, trained nurse abstractors at each of 40 participating hospitals collects detailed demographic and clinical data, including known risk factors for VTE, use of pharmacologic prophylaxis, and VTE events through 90 days after discharge for 760 patients annually. For this analysis, patients < 18 years of age or with length of stay < 1 day, obstetric or surgical patients, and patients admitted directly to the intensive care unit were excluded. VTE outcomes were determined by medical record review and follow‐up phone calls and included all proximal upper and lower extremity deep vein thrombosis and pulmonary embolism events. The Intermountain, IMPROVE, Padua, Kucher, and Caprini RAMs were applied to the HMS population and risk was classified as “at risk” or “low risk” based on the respective published cutpoints. Backward stepwise logistic regression was used to develop an HMS RAM. Each of the included risk factors was assigned one point and “at risk” was defined as a score of ≥ 2. To determine the predictive capabilities of the various RAMs, VTE events were regressed against each RAM and the respective model discrimination was assessed via the c‐statistic.
Results:
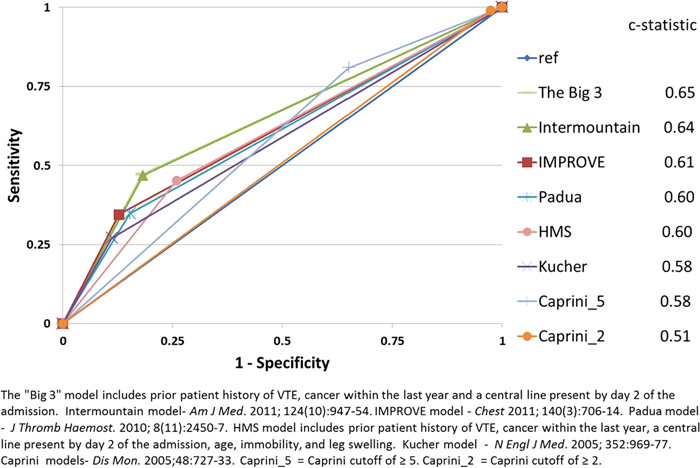
The performance of each of the RAMs was assessed on data collected on a total of 52,989 patients. In general, model discrimination was poor, with c‐statistics ranging from 0.51 – 0.65 (see Figure). The performance of our model (c‐statistic = 0.60) did not differ from the other RAMs assessed. A simple 3‐element RAM yielded the best model discrimination (c‐statistic = 0.65).
Conclusions:
The ability to predict VTE risk among a large cohort of hospitalized medical patients using existing and developed RAMs was limited. Parsimonious RAMs may have greater predictive ability and have the added advantage of facilitating risk assessment due to their simplicity. Additional work to determine which medical patients are at greatest risk for VTE and require appropriate thromboprophylaxis is warranted.