Background: Multidisciplinary rounds (MDRs) or discharge huddles in the hospital were developed to enhance safety and streamline discharge by improving communication between members of the patient care team. Despite efforts to coordinate care around a single brief daily meeting, multiple aspects of the patient’s care can change throughout the day. Keeping all members of the team updated is time consuming and information can be lost in the process. Current tools to help streamline communication among care team members do not fit the asynchronous reality of this real-time process. A structured checklist of specific tasks and patient factors related to discharge is also required to supplement MDRs, ensuring key elements are not overlooked. Incorporating the discharge checklist within the electronic medical record (EMR) would be ideal, as it would be accessible by all providers from anywhere in the hospital, kept in a secure environment, and can be reviewed in conjunction with clinical information that is pertinent to the patient’s anticipated discharge.
Purpose: The aim of the project is to create a discharge checklist within the EMR to facilitate near real-time updates in communication between a multidisciplinary care team, streamlining the discharge process, and ultimately decreasing unnecessary hospital days.
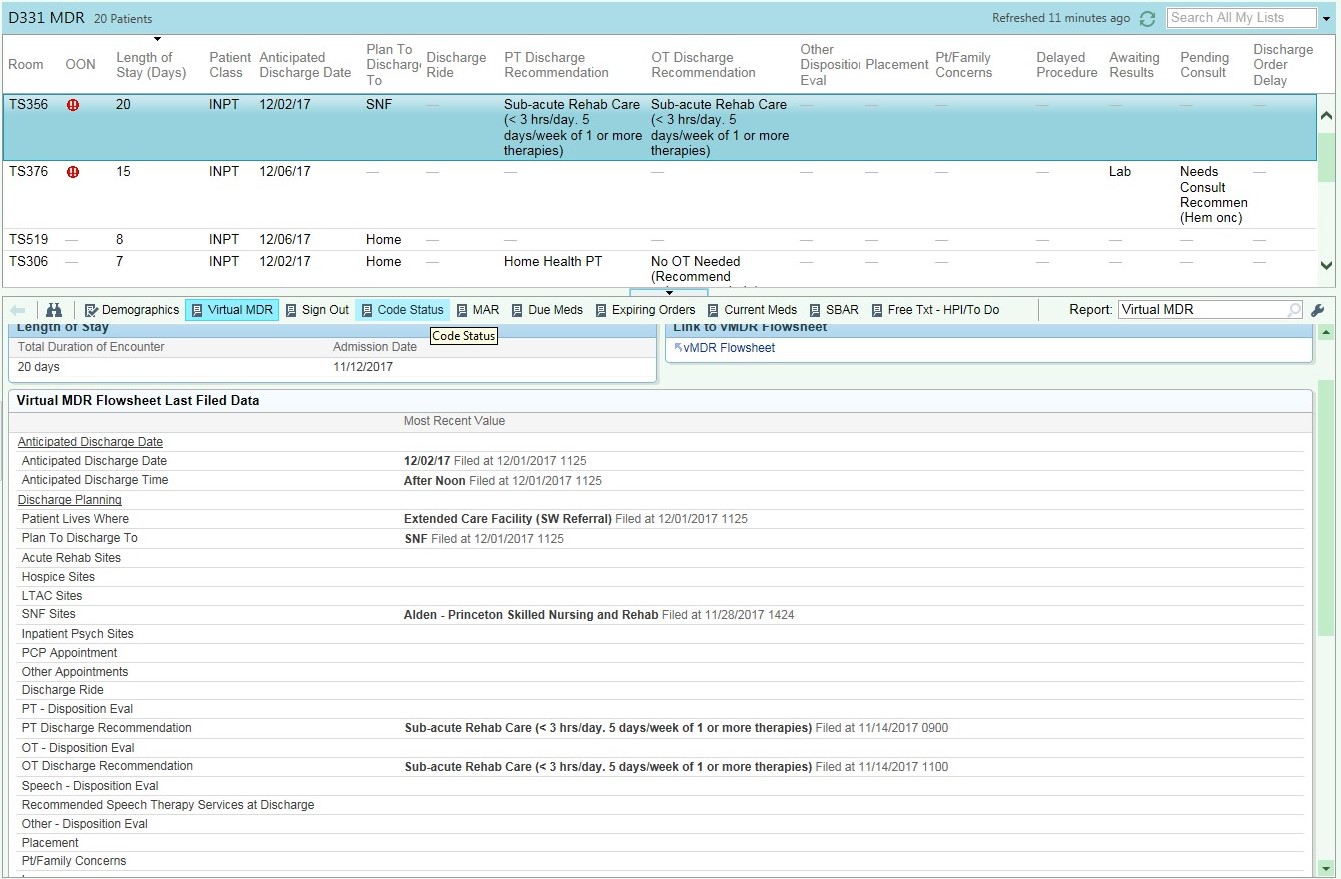
Description: A project team of clinicians, informatics experts, data analysts, and hospital leadership was assembled to create the initial checklist tool and determine how it could be incorporated into the EMR. The product of the workgroup, titled Virtual MDRs (vMDRs), is an interactive flowsheet within the discharge menu. Each element of the discharge checklist is listed in rows with specific buttons for the most likely selections (Figure 1). The tool can be viewed and altered by all care team members, including physicians, nurses, therapist, social workers, and case managers. Updates can be made and reviewed in multiple ways, including flowsheets, reports, and customizable columns into the patient lists (Figure 2), for better integration of various provider workflows. Implementation of vMDRs started with multiple pilot cycles to ensure all the necessary fields were included and easy to use. After a finalized product was developed, the tool was trialed by services managed by direct care hospitalists. Implementation was supported with informational sessions targeted at providers, social workers, and case managers, which identified the particular fields each team member is responsible for completing. Analysis of the tool’s impact is planned through review of commonly identified barriers, percentage of patients with completed vMDRs, as well as the outcome measure of patient length of stay.
Conclusions: The complicated process of safe and timely hospital discharge can be improved by an EMR embedded discharge communication checklist that allows for real-time updates by all care team members.
.jpg)