Case Presentation: A 39 y/o female with no significant past medical history and long term use of phentermine for weight loss presented to our hospital with complaints of transient right sided weakness and right sided facial droop lasting 30 min. At time of presentation, her symptoms had resolved completely and review of systems and physical exam were unremarkable with no focal deficits. Stroke team was consulted and patient was given full dose Aspirin (ASA), high intensity statin, and plavix. Imaging studies including CT head, MRA head and neck, MRI brain were unremarkable and TTE with bubble study was normal. CBC, CMP, and lipid profile were normal. She was diagnosed with TIA and remained asymptomatic and was discharged home with instructions to continue ASA, plavix, and atorvastatin and follow up with neurology outpatient.
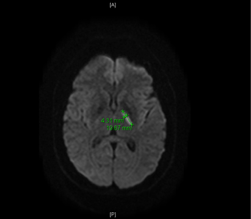
The next day, she presented again after waking up with expressive aphasia and right sided weakness. Vital signs were stable and physical exam was remarkable for dysarthria, decreased strength in right upper and lower extremities, and NIHSS of 4. Repeat imagining was ordered and MRI Brain on this occasion showed 2cm linear focus of acute ischemia within medial left basal ganglia and pt was diagnosed with ischemic stroke and per neurology was not a candidate for tpa. All other studies including MRA head and neck, venous lower extremity dopplers, and hypercoagulable work up were negative. She was given therapeutic lovenox, ASA, plavix, and lipitor and over the course of the next few days she clinically improved with resolution of expressive aphasia and improved right upper extremity weakness. She was discharged home with physical therapy, neurology follow up, and lipitor, ASA, and apixaban with instructions to stop smoking, avoid OCPs, and discontinue phentermine.
Her past medical history is only significant for headaches associated with her menstrual periods which resolve with use of PRN advil. She used no medications apart from the phentermine. She has a 2.5 pack year smoking history and drinks alcohol occasionally. She denied any history of clotting disorders, miscarriage, and does not use OCPs. She denied use of illicit drugs. Her family history was only significant for hypertension in her father and mother. She was using phentermine dialy for weight loss as prescribed by her PCP for a period of 2 years prior to presentation
Discussion: Phentermine is a psychostimulant and anorexiant, structurally similar to amphetamines, used medically as an appetite suppressant. It is most commonly known for it’s use with fenfluramine (fen-phen) which was pulled from the market due to significant cardiac adverse events. There are limited efficacy and safety data for phentermine and it’s approval for the management of obesity is limited to short-term use (≤12 weeks). A literature search only produced two case reports (from 1993) demonstrating possible association of phentermine use with ischemic stroke and ischemic colitis. To our knowledge there are no studies to date evaluating the risk of ischemic events with it’s long term use.
Conclusions: With the evergrowing popularity of weight loss drugs, it is imperative to evaluate the long term effects of this FDA approved drug. Our relatively young patient had very few risk factors for ischemic stroke. Amphetamine use has been associated with ischemic stroke due to it’s vasoconstrictive properties so randomized controlled trials evaluating the relationship between the pharmacologically similar phentermine for ischemic stroke are needed.