Background:
Many hospitals have tried to improve their medication reconciliation processes, with mixed results. Currently, there are insufficient data to guide hospitals in the best ways to improve their practices. In the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS), sites chose to implement one or more components from a multi-faceted toolkit. The goal of this analysis was to determine which components were associated with the greatest improvements in medication safety.
Methods:
Five U.S. hospitals participated in this quality improvement (QI) study between September 2011 and July 2014. With the guidance of trained mentors and using standard QI principles, each site implemented one or more of 11 intervention components. Sites were provided with an implementation manual and toolkit. Mentors conducted monthly phone calls and two site visits during the intervention period.
The primary outcome was the number of potentially harmful unintentional medication discrepancies per patient, measured in approximately 22 randomly selected patients per site per month during a 6-month baseline period and throughout the intervention. To determine the most effective components of the intervention, we categorized all QI activities conducted by any site by component, including date(s) of implementation. We analyzed the data using Poisson regression to detect sudden reductions in potentially harmful discrepancy rates temporally associated with each implementation of each intervention component across all sites.
Results:
We identified 668 patients on intervention units during the post-implementation period.
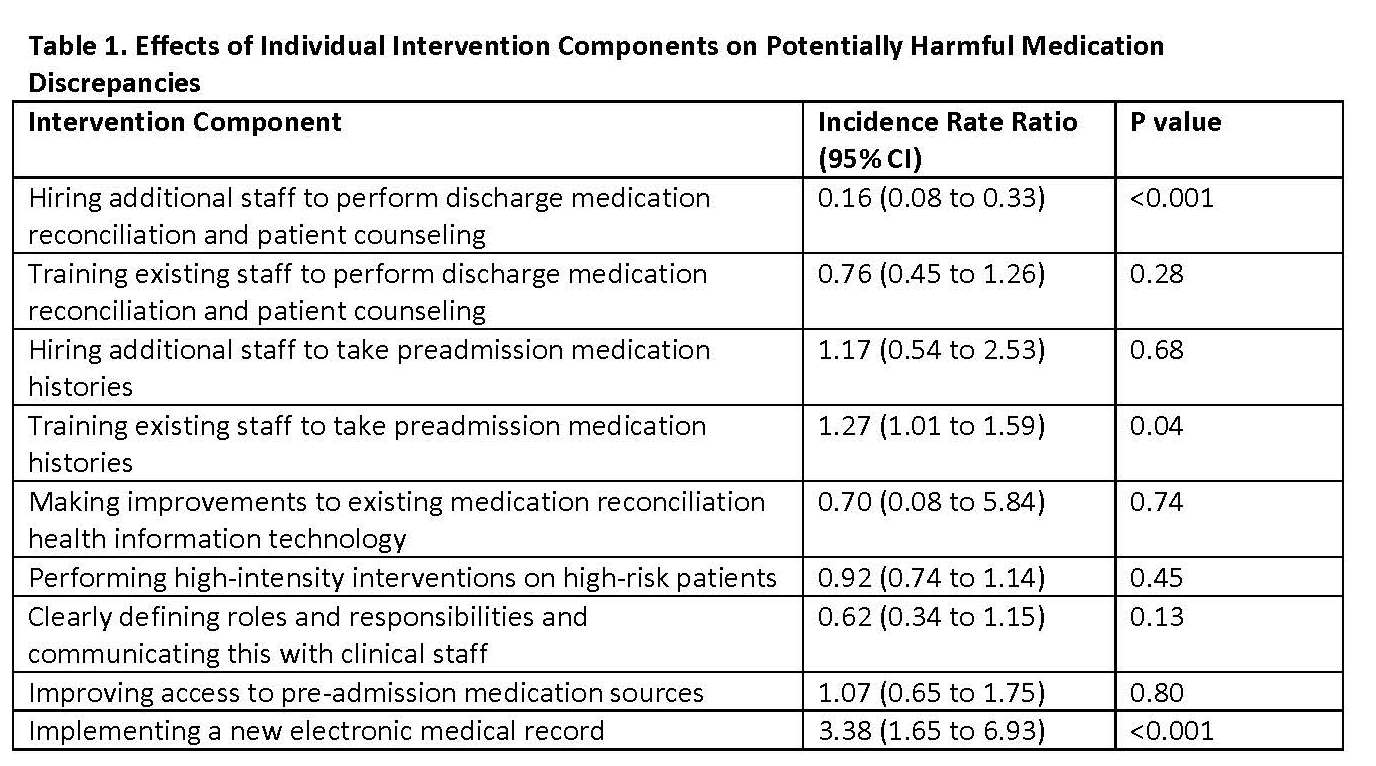
In on-treatment analyses, one intervention component was associated with significant reductions in potentially harmful discrepancies: hiring new staff (usually pharmacists) to assist with both medication reconciliation and patient counseling at discharge (incidence rate ratio 0.16 (95% CI 0.08 to 0.33)). Two components were associated with increases in discrepancy rates: training existing staff to take medication histories (IRR 1.27 (1.01 to 1.59)), and implementing a new electronic medical record (IRR 3.38 (1.65 to 6.93); Table 1).
Conclusions: We found that hiring additional pharmacy staff to assist with discharge reconciliation and patient counseling was the most effective component of a medication reconciliation QI program. Conversely, training existing staff to take medication histories was shown to increase potentially harmful discrepancies, perhaps because it leads to diffusion of responsibility or delays in hiring new staff, which could consolidate this role in a few well-trained personnel. Lastly, external factors, such as EMRs that are not designed and/or implemented optimally, were also shown to adversely affect discrepancy rates.