Background: There is little evidence that systemic improvements in hospital quality, safety, and cost of care have occurred in the U.S over the last 15 years despite calls to action and intense local efforts.1,2 Ongoing work by The Joint Commission shows that “best practices” from one hospital are unlikely to translate directly to another.3 Systematic refinements in improvement methods and infrastructure may be more likely to provide lasting solutions. Hospitalists at Emory University have developed a clinical microsystem model called an Accountable Care Unit (ACU)4 which structurally redesigns a hospital unit in an attempt to produce high-performing patient-centered teams which are actively managed and measured. Experience at a single, large, University hospital showed favorable results on process measures and mortality4.
Methods: We sought to determine if the model created at Emory could be implemented in a different care setting with similar results. In 2013, we redesigned a single hospital unit into a functioning ACU by: 1. Creating unit-based teams 2. Implementing daily Structured Interdisciplinary Bedside Rounds (SIBR) 3. Measuring unit level outcomes and 4. Creating a physician-nurse unit leadership dyad. The intervention unit was a 27-bed medical telemetry unit at a community teaching hospital. Using a time series analysis with case-mix matched controls from a large community hospital system, we examined the effects on mortality and 30 day readmissions during the 12 months prior to and 21 months after implementation. Costs per case and length of stay were tracked as balancing measures.
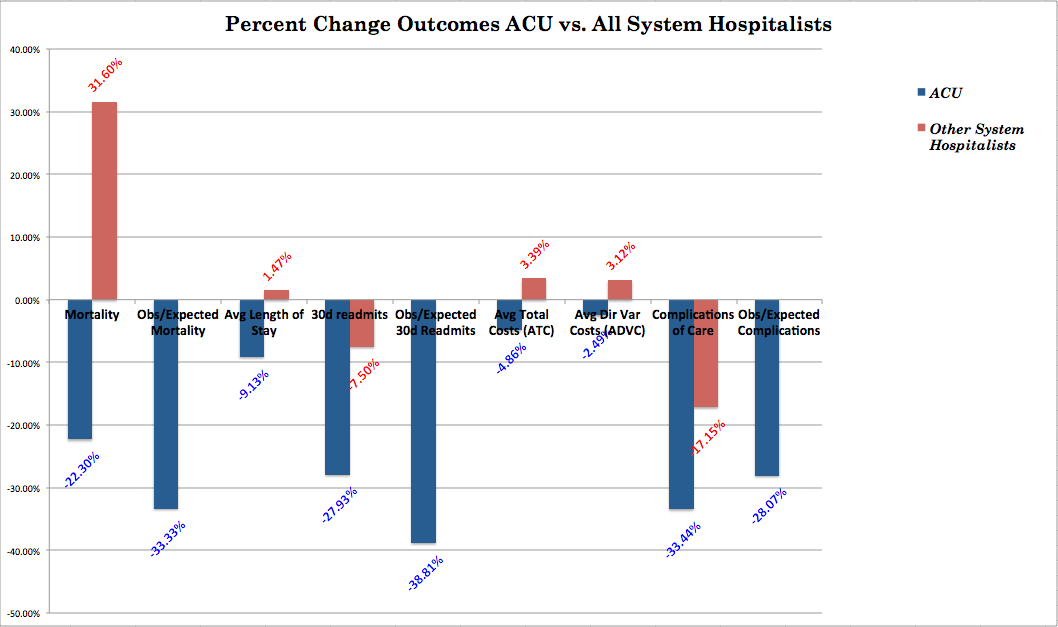
Results: Mortality rate on the ACU fell by 22.3% (1.84% to 1.43%) compared to an increase in mortality of 31.6% (1.90% to 2.50%) amongst all non-ACU hospitalist patient populations. Total 30-day readmission rate decreased 27.9% (17.58% to 12.67%) on the ACU and decreased 7.51% (15.05% to 13.92%) in the control group. Average length of stay (ALOS) decreased on the ACU by 9.13% (4.49 days to 4.08 days) while increasing in the control group by 1.05% (4.75 days to 4.80 days). Total costs decreased $464 per case (-4.86%) on the ACU while increasing $287 per case (+3.39%) in the control group. Process variance was substantially decreased. Depending on census assumptions, estimated cost savings attributable to decreased cost per case were up to $1,037,504 on a single unit over the 21-month study period.
Conclusions: An explicitly engineered clinical microsystem called an ACU is portable and has the potential to reliably provide improvements in mortality and readmission rates while decreasing length of stay and cost per case.