Background: Research suggests that ambulation in hospital settings can help prevent functional decline in patients. Early ambulation also contributes to better patient outcomes and decreased length of stay. The purpose of this study is to investigate patient perspectives to learn about factors that influence early ambulation and recommended amount of ambulation while in the hospital. A better understanding of these barriers and motivators is useful in developing effective interventions.
Methods: Data collection for this qualitative study occurred in 2016 at 354-bed hospital in a metropolitan area. A convenience sample of 6 patients completed a semi-structured, in-person interview. An interview guide was used to explore: patient adherence to recommended amount of ambulation, barriers to mobility, family member influence, and suggestions for how mobility can be increased. The interviews were all recorded and transcribed verbatim. This study used a grounded theory approach using thematic analysis to analyze interview transcripts.
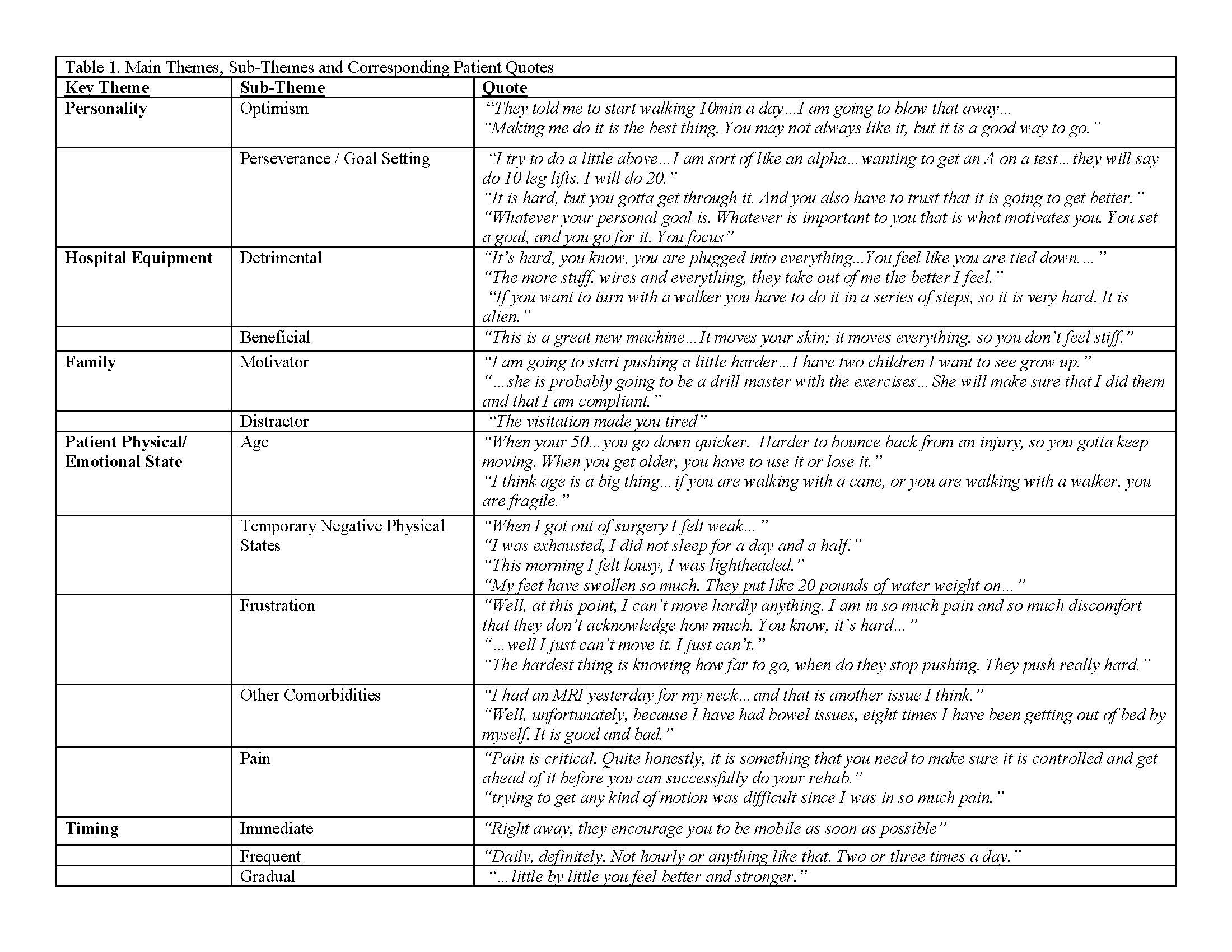
Results: Five males and one female were interviewed, ages ranging from 56-74 years old. Three of the patients were Cardiac post-surgical patients. The other three patients were Orthopedic post-surgical patients. Six main themes were identified: (1) Personality, (2) Hospital Equipment, (3) Family, (4) Patient Physical and Emotional State, (5) Timing, and (6) Patient Education and Communication. There were several sub-themes within each key theme. Personality included: optimism and perseverance/goal setting. Hospital Equipment included: detrimental and beneficial. Family included: motivator, distractor. Patient Physical and Emotional State included: age, temporary physical states, frustration, other comorbidities, and pain. Timing included: immediate, frequent, and gradual. Education and Communication included: multi-modal communication, education, and expectations.
Conclusions: In this study, patients described different barriers and influences associated with ambulation in a hospitalized setting. Positive personality traits, supportive family members, appropriate patient education/communication, and proper timing are all motivating factors in mobility. However, negative personality traits, apprehensive family members, frail physical/emotional state, pain, and lack of education/communication are all barriers. Hospital equipment, can be a motivator or a barrier depending on the context. Next steps include further investigating healthcare team perspectives on motivators and barriers for mobility as well as developing interventions to enhance incentivizes and decrease obstacles.