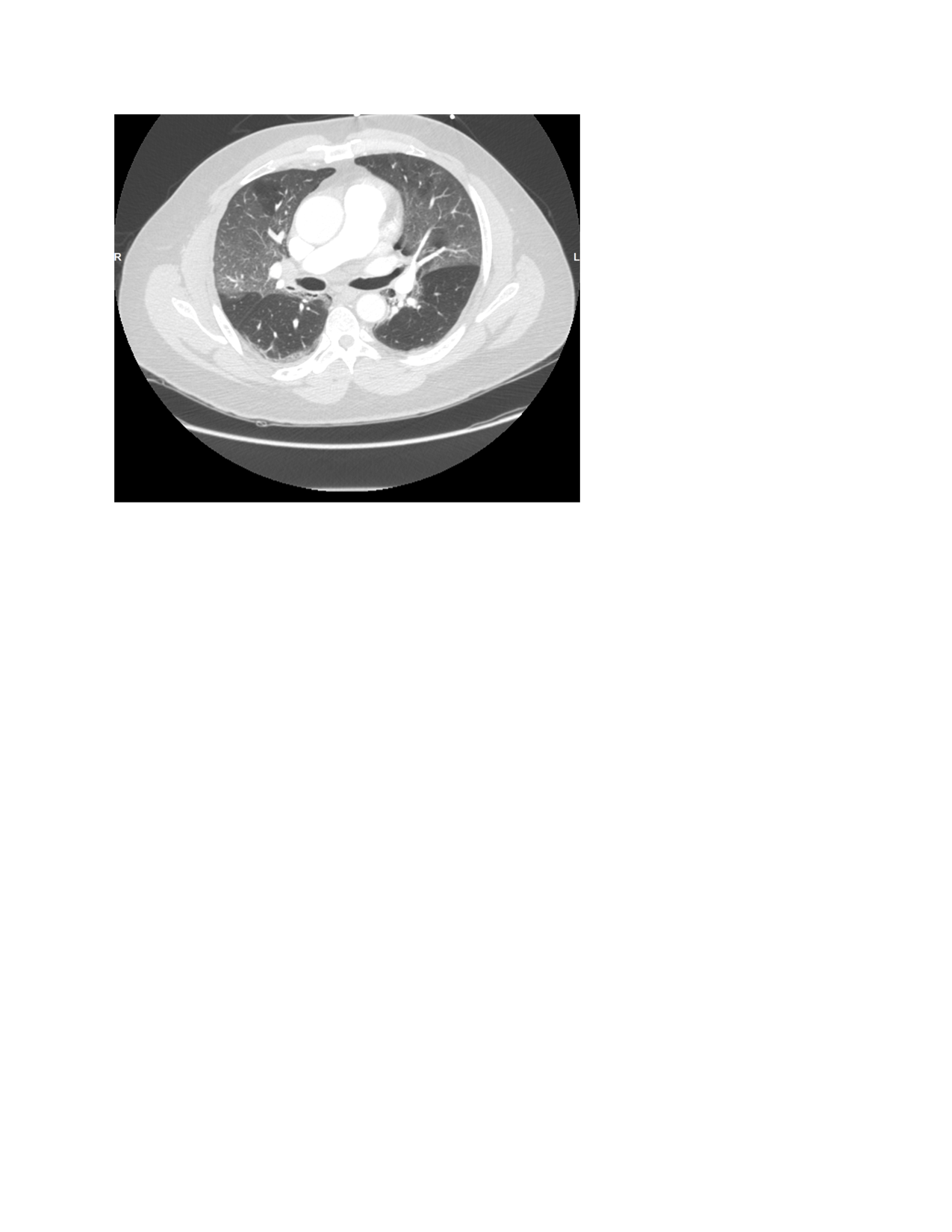
Case Presentation: A 59-year-old male with a past medical history remarkable for obesity, asthma, and anxiety sought medical attention for the chief complaint of dyspnea for approximately 10 days. Computed tomography with angiogram of the thorax on admission was negative for any pulmonary emboli, but did demonstrate central and peripheral ground glass opacities throughout both lungs. He subsequently tested positive for COVID-19. He was admitted to the ICU for progressively worsening hypoxemic respiratory failure. He was noted to have an elevated d-dimer of 0.5 mg/L and therapeutic lovenox dosing was initiated on day 1 of his hospitalization. He was also initiated on remdesivir for which he completed a total of 5 days and dexamethasone 6mg. In addition, he was started on azithromycin and ceftriaxone, although infectious work up for any possible superimposed bacterial infection was negative. On day 5 of hospitalization he developed dysarthic speech, left-sided facial droop, left sided paralysis and sensory deficits. A code stroke was called and computed tomography with angiogram of the head and neck demonstrated an occluded superior M2 segment and multifocal distal occlusions in the inferior M3 segment. He was also noted to have acute/new bilateral upper lobe pulmonary emboli. He received tissue plasminogen activator and was subsequently intubated prior to undergoing partial thrombectomy performed by interventional neuroradiology. Unfortunately, despite the aforementioned treatment modalities, he continued to decline. Inflammatory markers remained elevated throughout his stay- reaching maximum levels- high sensitivity d-dimer 1.69 mg/L, ferritin 2,370 ng/mL, sedimentation rate 96 mm, c-reactive protein 15.5 mg/dL and LDH 641U/L. He remained on therapeutic dosing anticoagulation. Several days later the patient went into cardiac arrest and ultimately expired.
Discussion: The novel coronavirus, SARS-associated coronavirus (SARS-CoV) is known to cause the severe acute respiratory syndrome (SARS). Mortality of this disease has been strongly associated with hypoxemic respiratory failure/ARDS; however, thromboembolic complications are becoming an increasingly recognized contributor of mortality. Klok et al., reported a thrombotic incidence of 31% in patients admitted to the intensive care unit (ICU) with COVID-19 pneumonia. It is now recommended that all patients with respiratory failure secondary to COVID-19 receive prophylactic anticoagulation dosing. In addition, a mortality benefit has been shown with the use of therapeutic anticoagulation dosing. Several possible mechanisms have been proposed to explain the hypercoagulability associated with this condition, such as, the development of reactive antiphospholipid antibodies, excessive complement activation, and even disseminated intravascular coagulation (DIC). In addition, several articles have suggested that elevated D-dimer levels may be secondary to elevated serum plasmin levels.
Conclusions: This case highlights the importance of early anticoagulation in patients with respiratory failure secondary to COVID-19 infections, but also to increase awareness and provide warning that even therapeutic anticoagulation may not be enough to prevent thromboembolic complications from the increased hypercoagulability associated with this disease state. Further understanding of the pathogenesis of this disease is required in order for us to more efficiently guide treatment decision making.