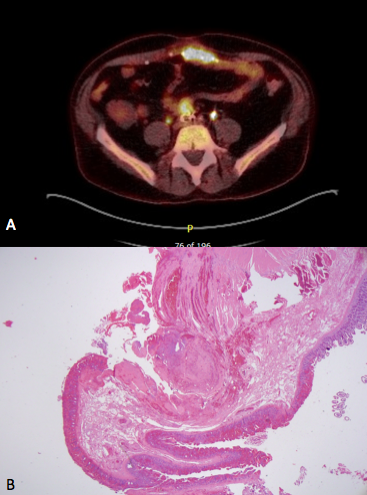
Case Presentation: A 67 year-old man with history of transient ischemic attack, coronary artery disease, and peripheral artery disease status post aorto-iliac graft in 1994 presented with intermittent fevers, chills, and intense rigors. Symptoms started following a dental procedure 6 months earlier after which he was diagnosed with streptococcus anginosus bacteremia. Continued fevers prompted trans-esophageal echocardiography, cross sectional imaging, followed by a tagged white blood cell scan that were all non-revealing. Patient was treated with a long course of Vancomycin with recurrence of symptoms as soon as antibiotic therapy was interrupted. He was thus repeatedly hospitalized and eventually presented to our institution with the same symptoms. Vital signs on presentation were within normal limits with a benign physical examination. Laboratory evaluation revealed mild leukocytosis at 11 k/uL, hemoglobin of 10.2 g/dL, and platelet count of 252 k/uL. Complete metabolic panel was normal. Inflammatory markers were elevated with a CRP of 6.3 mg/dl and an ESR of 47 mm/hr. Urinalysis and chest radiograph were normal. Two sets of blood cultures turned positive for citrobacter and another two sets grew Enterococcus Faecalis. Patient was started on antibiotics and evaluation for an infectious source included an echocardiography and a CT angiogram both of which were negative. With the concern for a graft infection, a PET scan was done and showed focal FDG uptake at the interface of a small bowel loop and the aorto-iliac graft (Panel A; Figure 1). With the high clinical suspicion, patient was taken to the operating room where enteric content was identified within the graft along with a hole in the small bowel raising suspicion for an aortoenteric fistula. Pathology of the resected bowel segment demonstrated an inflamed and ischemic transmural defect consistent with an enteric fistula (Panel B, Figure 1). Following surgery, patient finished a 6-week course of antibiotics without recurrence of the symptoms.
Discussion: Despite the low incidence of endograft infections (0.4-3%), mortality rates approach 25%. While most cases tend to occur within 3 months of surgery, this serious complication can happen many years afterwards as our case demonstrates. Diagnosis hinges on a high index of suspicion and whereas most cases can be diagnosed with an enhanced CT scan, a minority of cases might not be apparent. In these situations where the routine imaging do not support the high clinical suspicion, more sophisticated diagnostic modalities with higher sensitivity might be useful to reach the right diagnosis.
Conclusions: This case highlights the importance of interpreting diagnostic studies only in the context of the pretest probability. If the clinical suspicion is high then hospitalists should exhaust all diagnostic options before ruling out a potentially deadly diagnosis such as a graft infection or an aortoenteric fistula.