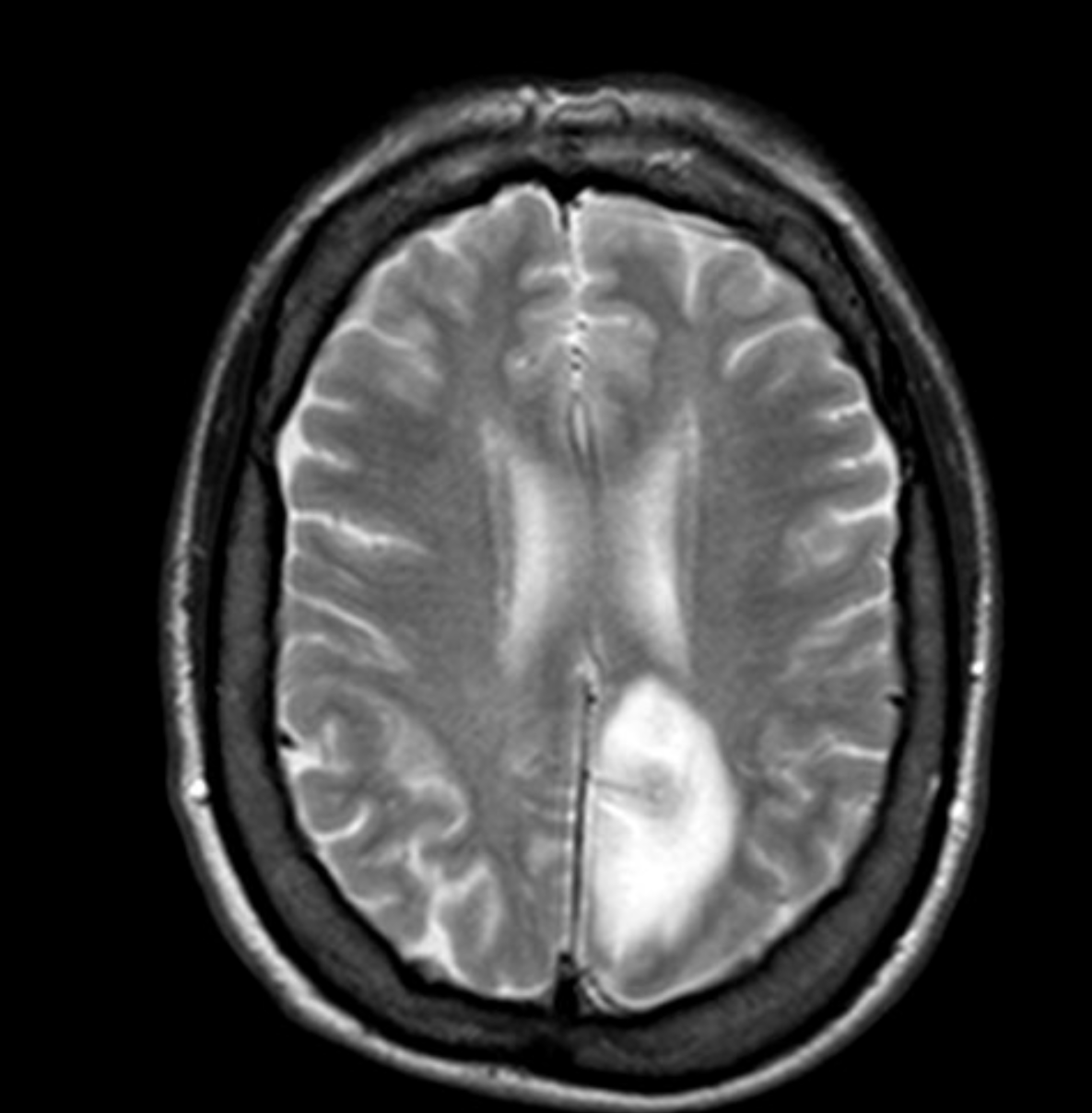
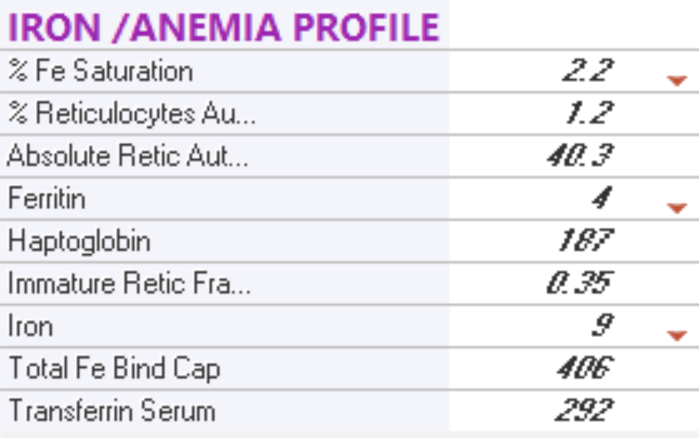
Case Presentation: We present a case of a 37-year-old female with a past medical history of cerebral palsy and iron deficiency anemia due to heavy menstrual periods who presented with right-sided leg weakness for a few hours. Upon the patient’s arrival to the emergency room a stroke code was called. A CT scan of the head showed a hypodensity in the left posterior cerebral artery territory. A CT angiography of the head and neck showed patent vessels. The patient did not end up getting tPA as she was out of the time window for tPA administration. Basic initial laboratory tests were significant for a platelet count of 1303 k /uL. Hemoglobin of 6.2 g/dL. Hematocrit of 21.3% and MCV of 63 fL. Decision was made to undergo platelet pheresis due to symptomatic thrombosis. Her platelet count post procedure dropped to 736 k /uL. The patient was started on Aspirin.Further workup for thrombocytosis and anemia was consistent with severe iron deficiency. Ferritin was 4 ng/ml. Iron saturation was 2.2% and serum Iron was 9 ug/dl. An MRI of the brain showed Abnormal signal intensity within the left parietal parasagittal region extending to the vertex. A lipid panel was essentially normal with a total cholesterol of 96 mg/dl and an LDL level of 48 mg/dl. Then the patient was discharged on day 3 in stable condition, she received 2 treatments of 200 mg IV iron sucrose and was discharged on iron supplement. Testing was done for JAK2, CALR, MPL mutations which later came back negative.
Discussion: Thrombocytosis can be divided into two etiologies: reactive and autonomous (neoplastic) overproduction. Reactive causes of thrombocytosis such as infection, inflammation, blood loss, hemolysis or iron deficiency usually cause less severe thrombocytosis. Furthermore, thrombotic and bleeding events are much less likely to occur with reactive thrombosis than autonomous thrombosis. However thrombotic events were occasionally reported in iron deficiency anemia. In our case, we described a thrombotic event which is a cerebrovascular accident in the left posterior cerebral artery territory solely caused by reactive thrombocytosis from iron deficiency anemia. the patient had a negative workup for other causes of thrombocytosis as her JAK2, CALR and MPL mutations study were negative. She did not have an active infection and she did not have any clinical or laboratory signs of occult malignancy. Her lipid panel was within normal limits and she did not have any direct family history of CVA making other causes of stroke much less likely.
Conclusions: It is easy to overlook iron deficiency anemia in hospitalized patients especially if the cause of hospitalization is not related to the anemia itself. However, hospitalists can play an imperative role in identifying and starting the treatment of iron deficiency anemia to avoid rare but potentially catastrophic consequences such as our patient. When iron deficiency anemia is identified in the hospital, the hospitalist can initiate the treatment with IV iron in the hospital if indicated, discharge the patient with the required iron supplement and arrange for appropriate follow up with the patient’s primary care physician in the outpatient setting.