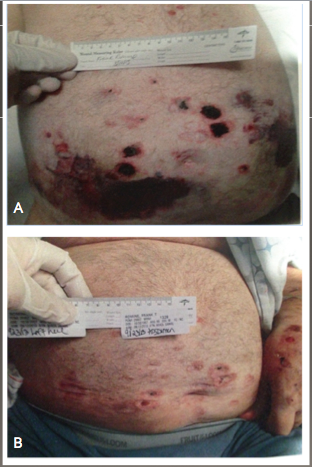
Case Presentation: A 55-year-old man with gastroesophageal reflux disease and prostate cancer status post radical prostatectomy presented with a 3-year history of non-healing skin ulcerations. He was initially diagnosed with vasculitis and started on immunosuppressive therapy. Skin lesions worsened despite high dose steroids and different immunosuppressive medications (methorexate, mycophenolate, azathioprine, cyclophosphamide). On presentation, skin examination showed large ulcerations over the abdomen (Panel A; Figure 1) with multiple tendon-deep lower extremity ulcerations. Medications included 60 mg of prednisone daily and Cellcept 10mg BID. Laboratory tests showed a hemoglobin of 10 g/dL, platelets 94K/μL. Complete metabolic panel was normal except for a low total protein at 4.7g/dL with an albumin of 2.7g/dL. Urinalysis with microscopy was normal. Skin biopsy showed leukocytoclastic vasculitis (LCV). Infectious workup including HIV, remote hepatitis panel, CMV, EBV, HSV, syphilis, and fungal battery were all non-revealing. Echocardiography showed no evidence of endocarditis. Immune workup including ANA, ENA panel, rheumatoid factor, complement levels, C and P ANCA, cryoglobulins, and cryofibrinogens were negative. CT chest/abdomen/pelvis was negative for occult malignancy. Serum protein electrophoresis revealed a low level M protein in the IgA and lambda regions consistent with a monoclonal gammopathy. Bone marrow biopsy showed a hypo-cellular marrow (30%) with evidence of a plasma cell neoplasm, lambda monotypic, accounting for 5% of the total cellularity. After much discussion regarding the significance of this finding, patient was started on Velcade (Bortezomib). He finished 2 cycles before transitioning to a long-term acute care hospital. Upon discharge, Mycophenolate was stopped and prednisone was being tapered. Follow up after 6 weeks showed an impressive improvement in the skin lesions (Panel B; Figure 1).
Discussion: LCV is a term that refers to small vessel vasculitis of the skin. An underlying primary vasculitis is generally present in only 4-6% of cases. Secondary etiologies such as chronic infections, medications, connective tissue diseases, and malignancy account for the majority of cases of LCV. When confronted with a case of LCV, an exhaustive evaluation for an underlying etiology should be performed. While steroids and immunosuppressive medications are the mainstay of treatment of primary vasculitides, they might carry significant risk with other diagnoses, such as progression of infection or malignancy. As such, an accurate diagnosis is integral to the proper therapeutic intervention.
Conclusions: When caring for patients admitted with worsening vasculitic skin ulcerations, hospitalists need to question the underlying diagnosis and the steroid use when the response to escalating doses appears suboptimal.