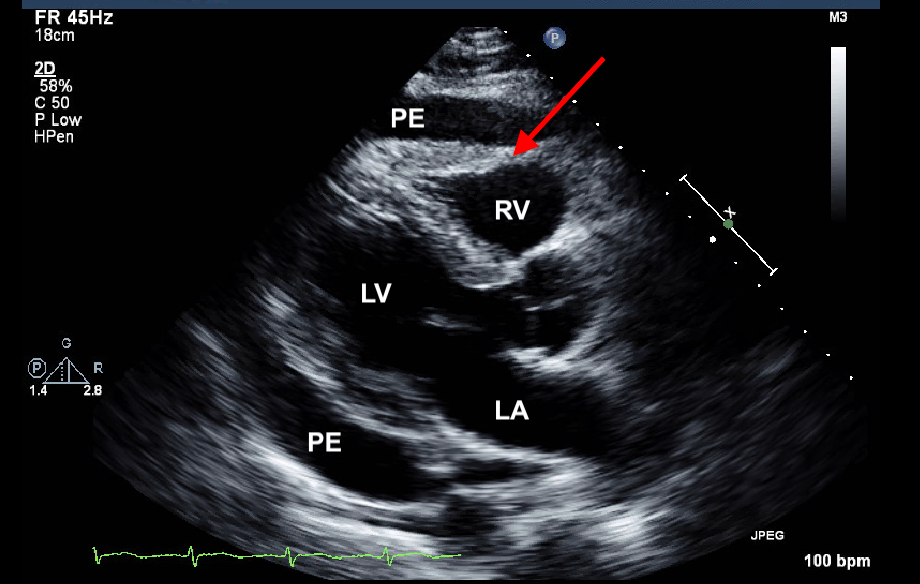
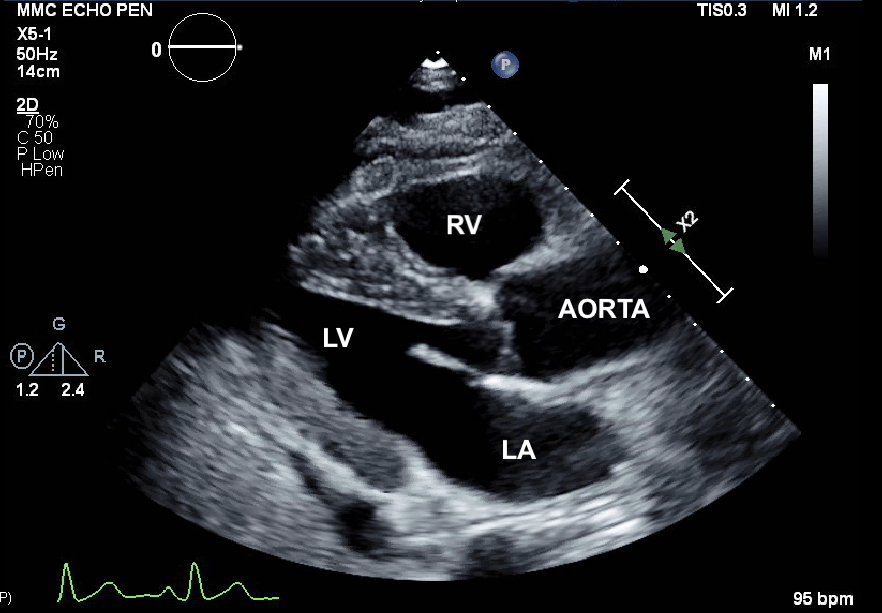
Case Presentation: A 46-year-old male with history of hypertension and Covid-19 illness seven months ago presented to the ER complaining of left flank pain for the past six days.Pain was described as sharp, constant, initiating on his left flank and radiating to the upper abdomen. He denied dysuria, hematuria, fevers, sick contacts, or trauma. No history of renal lithiasis. Reported dyspnea since Covid-19 illness associated with progressive orthopnea. No chest pain. On physical exam, BP 129/82 mmHg, HR 110, 37.3°C, RR 18, SpO2 96%. No jugulo-venous distention. Heart sounds were rhythmic. Clear breath sounds. Soft abdomen and no costovertebral angle tenderness. CBC, BMP and LFTs were normal; cardiac enzymes (CK 385 U/L, troponin I <0.01 ng/mL); ESR/CRP elevated. SARS-CoV-2 IgG positive and PCR negative. EKG with normal sinus rhythm. Urinalysis was negative for UTI and microscopic hematuria. CXR reported cardiomegaly. CT abdomen/pelvis was done to rule out genitourinary pathologies and revealed a pericardial effusion. No evidence of hydronephrosis or calculus.Echocardiogram reported a large pericardial effusion with diastolic right heart collapse (Fig. 1). Given hemodynamic compromise, pericardiocentesis under ultrasound and fluoroscopic guidance was performed with removal of 950ml of fluid leading to good right heart expansion (Fig. 2). Patient reported complete resolution of left flank pain after pericardiocentesis.Pericardial fluid microbiology studies were negative. The patient was discharged home in stable condition.
Discussion: Pain is the main chief complaint on presentation to the ER (1). Flank pain is often below the rib and above the ilium, resulting from stimulation of nerve endings upon distention of the ureter or renal capsule. Similar pain is sometimes caused by extra-urinary abnormalities including chest diseases (2). Pericardial pain tends to be sharp and retrosternal, frequently being part of systemic diseases. Infectious etiologies represent a common cause; however, little is known on post Covid-19 complications (3,4). Cardiac tamponade occurs when fluid accumulation in the intrapericardial space is sufficient to alter cardiac filling (5). Because of its lower pressures, the right heart is most vulnerable to compression, representing the earliest sign of hemodynamic instability; and if untreated may lead to shock or death (6,7). The gold standard treatment is pericardial drainage (8). Medical management is ineffective in compromising effusions and should be used only while arrangements are made for pericardial drainage (9). A late complication and rare pain presentation may be related to this subject Covid-19 history. There are multiple cases of myopericarditis and pericardial effusions associated with SARS-CoV-2 infection without a clear mechanism of injury(10).
Conclusions: Pericardial effusion is a life-threatening disease that can lead to hemodynamic compromise and obstructive shock. Clinical signs and symptoms of pericardial diseases have been well described in the literature; however, associated left flank pain is a rare chief complaint on the initial presentation. Gold standard treatment with therapeutic pericardiocentesis showed complete resolution of left flank pain post-procedure. It is uncertain if previous Covid-19 infection could alter nociceptors leading to atypical cardiac pain presentations, further studies and reviews are needed.