Case Presentation: A 75 year-old man with recently diagnosed bladder cancer presented with fever and dyspnea, one month after a laparoscopic cystectomy, radical prostatectomy, lymph node dissection, and urinary diversion via ileal conduit.
On arrival, he was febrile to 38.4 C, heart rate of 110 bpm, tachypneic on 2L supplemental oxygen. His abdomen was nontender to palpation. Labs were notable for a WBC count of 13.6 (92% PMNs) and a creatinine of 2.0 mg/dL (up from baseline of 1.0 mg/dL). Chest X-ray showed no evidence of pneumonia. Two sets of blood cultures were obtained and he was started on broad-spectrum antibiotics with piperacillin/tazobactam and vancomycin.
His blood cultures turned positive for bacteroides fragilis and he developed worsening abdominal distension. A CT abdomen/pelvis was notable for ascites without an organized fluid collection. A 3-liter paracentesis revealed cloudy yellow fluid that contained 3,971 WBC/cubic mm, 74% of which were PMNs and 12% lymphocytes. Ascites cultures were negative. Serum ascites-albumin gradient was >1.1. A liver ultrasound was unremarkable with no evidence of a portal vein thrombosis, portal hypertension, or Budd-Chiari. An echocardiogram was unremarkable. Further imaging was performed to evaluate for a bowel or urinary leak given his recent surgery that revealed no extravasation of contrast from his ileal conduit, or from the bowel re-anastomosis. A repeat paracentesis was performed that showed a normal glucose, amylase, bilirubin, LDH, creatinine, BUN, and triglycerides.
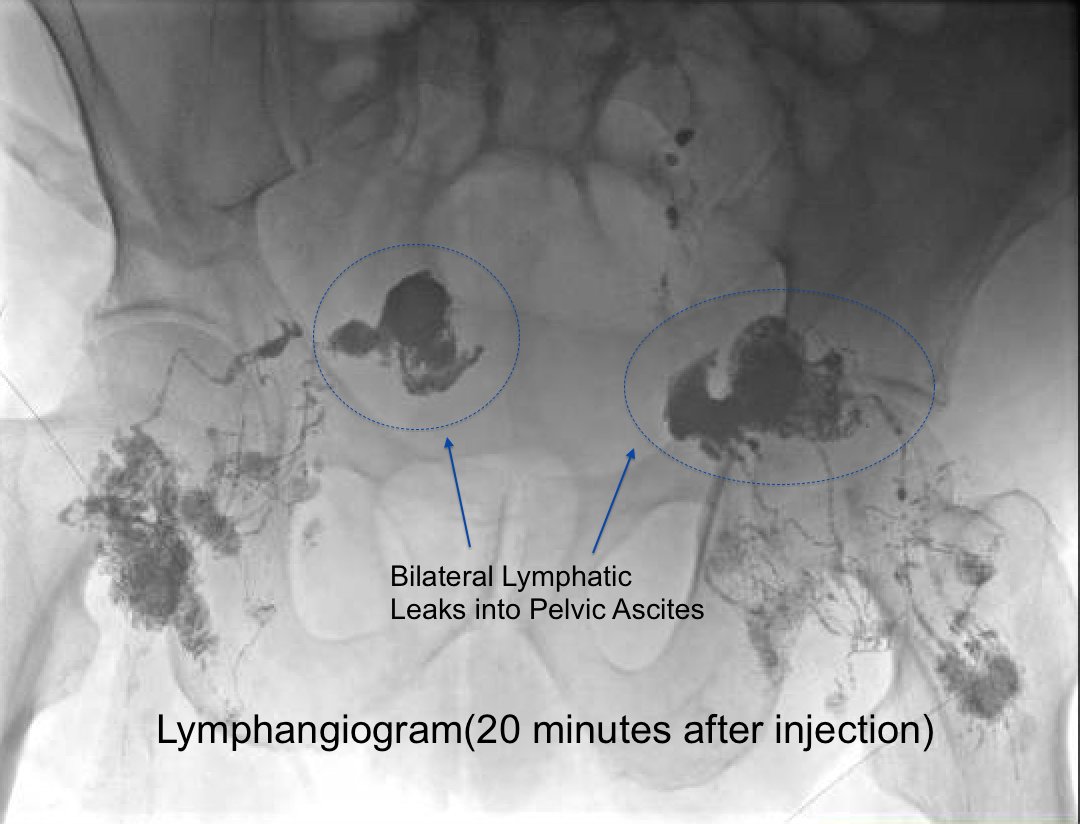
Despite antibiotics, patient continued to have recurrent ascites. A liver biopsy showed no abnormalities. Despite the non chylous appearance of his fluid, he underwent pelvic lymphangiography that revealed pooling of contrast in both hemipelves suggestive of a lymphatic leak. He underwent lymphatic gluing by interventional radiology with eventual resolution of ascites and clearance of his infection.
Discussion: Lymphatic injury is a rare complication of retroperitoneal lymph node dissection. When it does occur, and if ascites is present, the fluid analysis is typically chylous. Management is usually focused on altering the diet, bowel rest, and sometimes parenteral nutrition. Lymphatic injury in the pelvis, though rare, is most commonly associated with complications of surgeries related to testicular cancer and retroperitioneal lymph node dissection. There are no case reports in the literature of accumulation of non-chlyous ascites secondary to lymphatic injury after a cystectomy.
The cisterna chyle of the lymphatic system is the structure that represents the transition from chylomicron poor and rich fluid. The characteristics of the lymphatic fluid superior to this structure are always high in triglycerides as it accumulates chylomicrons. As our patient’s injury occurred inferior to the cisterna chyle, his ascites was not triglyceride rich, and was therefore not milky in appearance, and the initial suspicion for lymphatic injury was low.
Conclusions: Hospitalists should be aware of lymphatic ascites as a cause of recurrent ascites after pelvic surgery. They should be aware of the important clinical ramifications of injuries below the cysterna chyle, most importantly that lymphatic injury could be a cause of recurrent ascites, even if the fluid does not have a high triglyceride count. They should be aware of the advanced diagnostic and therapeutic interventions that can resolve lymphatic leaks and thus eliminate a source for potential infections such as bacterial peritonitis.