Background: Communicating to physicians about electronic health record (EHR) software updates is important for maintaining clinical workflow and preserving patient safety. However, reaching providers with mass e-mails is challenging; the optimal strategy for educating providers about EHR updates remains unclear.
Purpose: Modify our communication strategy to improve inpatient physicians’ understanding of EHR software updates.
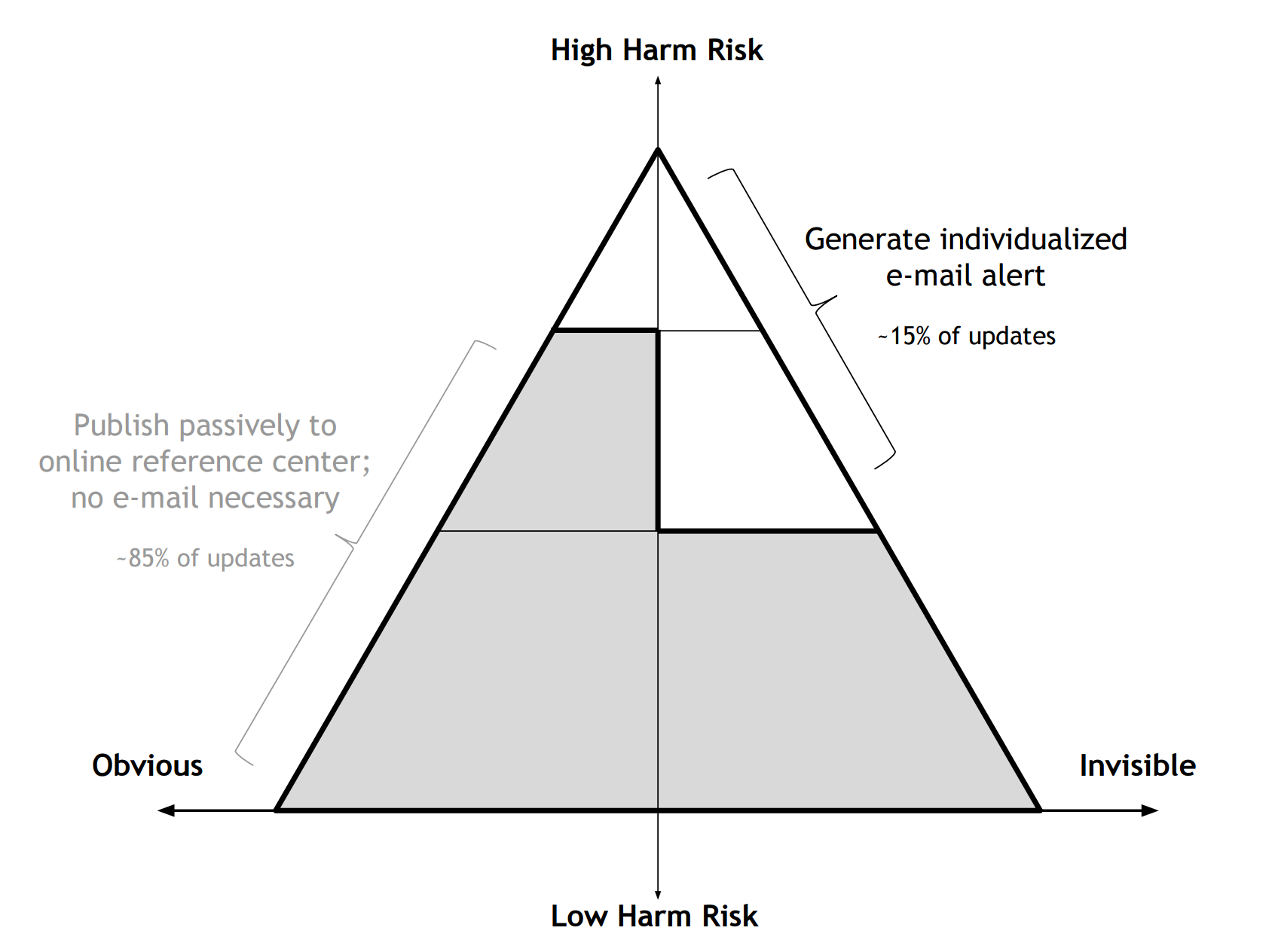
Description: To first understand why information about EHR updates had been failing to reach physicians we distributed a survey to 263 Medicine, Pediatrics, Neurology, and Surgery residents at our large academic institution; 42 responded (16%). Very few respondents (1/42) typically read mass e-mails about EHR updates. Accordingly, few (4/42) were aware when EHR updates occurred. Most (30/42) cited receiving frequent updates irrelevant to their work as a major reason for not reading the e-mails. Based on these results we designed a two-pronged approach to increase the salience of communications about EHR updates: 1) eliminate superfluous messaging to reduce notification fatigue and 2) send messages only to individuals affected by each update. To eliminate superfluous messaging, we developed a new framework (Fig. 1) to guide decisions about which EHR updates warrant outgoing communications. We now score updates on two axes: risk of patient harm if providers are unaware, and obviousness of the update to providers. We then send communications only about high-harm, non-obvious (invisible) changes (e.g., “New Tracheotomy Speech Valve Workflow”), and refrain from sending communications about low-harm, obvious changes (e.g., “New Question Added to Intake Form”). This stratification scheme eliminates the need for ~85% of outgoing communications, as assessed from a random sample of updates; the remaining ~15% thus, in theory, receive more attention. Applying this framework has allowed our EHR training team to reduce the number of topics covered in educational efforts for an upcoming EHR system upgrade from 77 topics to just 20. The second prong of our approach is sending updates only to individuals affected by each change. We developed a workflow enabling us to identify individuals that have recently used a given feature (e.g., physicians placing an order for a specific medication) by analyzing a database of user activity. We then generate notifications only to those users, identifying recipients by name and explaining why they are receiving a personalized message based on past activity.
Conclusions: Responding to a need and specific feedback from providers we designed a strategy to curate communications about EHR updates for individual providers, with the aim of improving their understanding of changes to their EHR-based clinical workflow.