Background: Spontaneous bacterial peritonitis (SBP) is a life-threatening infection in patients with cirrhosis. Depending on the clinical setting, the prevalence and mortality rates of SBP in cirrhosis range between 1.5-30% and 10-46%, respectively. The purpose of this study was to assess the yearly trend in SBP prevalence, length of stay and mortality among hospitalized cirrhosis patients from the years 2006-2013 using a US inpatient database.
Methods: National Inpatient Sample, which is a large inpatient US database sponsored by Agency for Healthcare Research and Quality, was used to identify patients ≥18 years with SBP (ICD-9-CM-code-567.23) and cirrhosis (ICD-9-CM-code-571.2, 571.5, 571.6) from the years 2006-2013. Prevalence of SBP in cirrhotic patients was calculated, along with mortality and length of stay (LOS). STATA version 13.0 (College Station, TX) was used for all analyses. Joinpoint regression software was used to test the annual trends in terms of annual-percentage-change (APC).
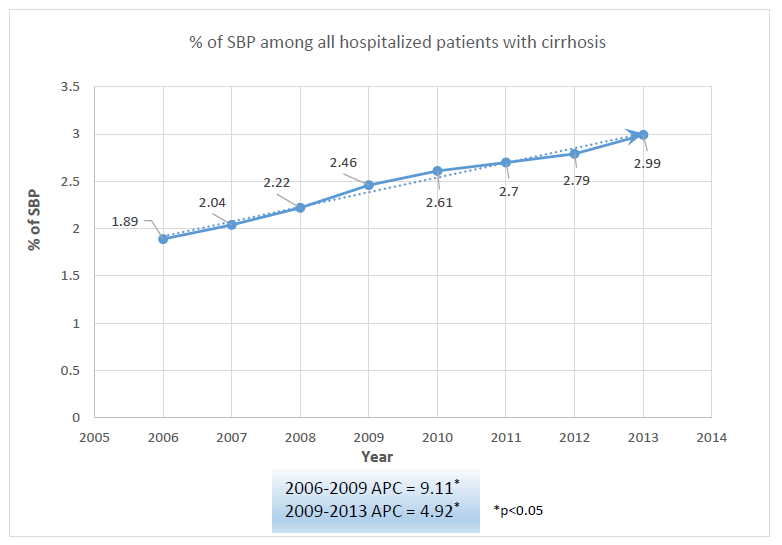
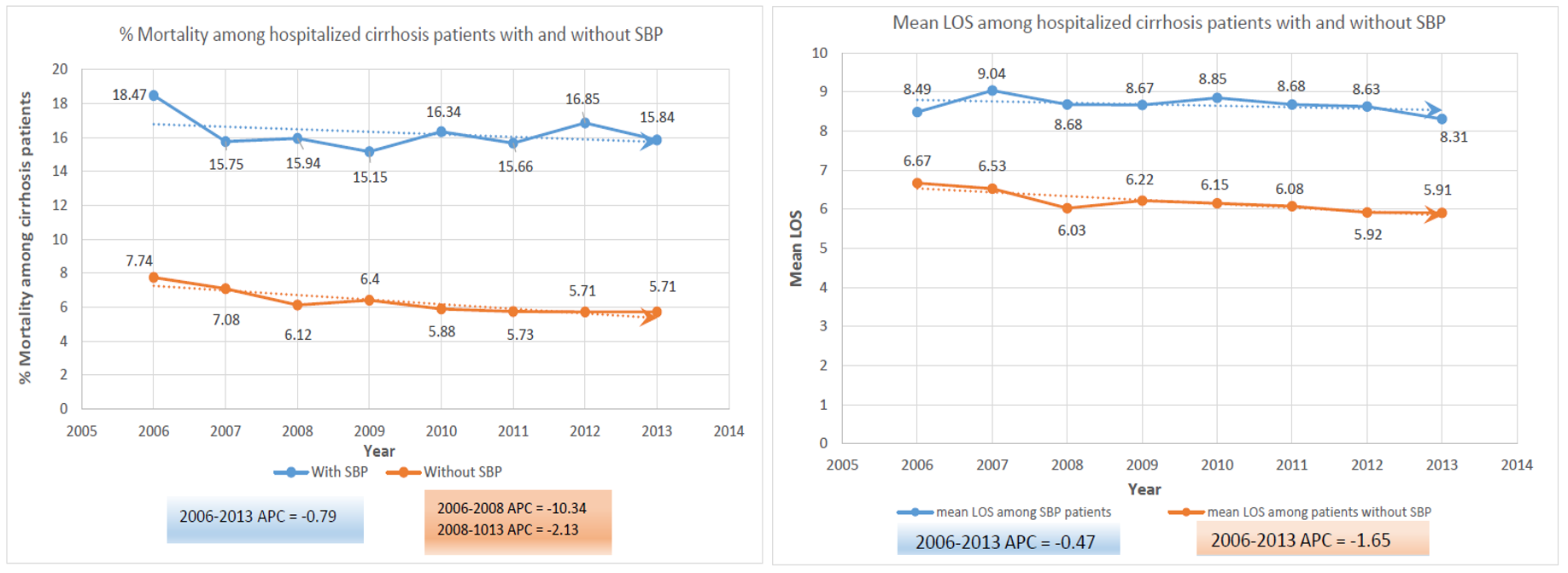
Results: An estimated total of 4,067,963 hospital discharges with cirrhosis were identified, among which 101,891 were identified to have SBP. A significant increase in SBP was noted from the years 2006-2009 with an APC of 9.11, followed by a further increase from 2009-2013 with an APC of 4.92, p<0.05 (Figure 1). SBP-associated mortality and LOS were only slightly reduced with APC -0.79 and -0.47, respectively. In 2013, mortality and mean LOS among hospitalized cirrhosis patients with SBP were 15.84% and 8.31 days, respectively, compared to 5.71% and 5.91 days in those without SBP (Figure 2).
Conclusions: SBP continues to rise despite multiple strategies including diagnostic bedside-paracentesis in all new or worsening ascites and prophylactic antibiotics for high-risk-cirrhosis-patients. This could be due to an increasing trend of cirrhosis, higher SBP diagnosis-rates, ineffective prophylaxis or an excessive PPI use which has been reported to increase bacterial translocation. With increased incidence, challenges in treatment have been observed. The emergence of multi-resistant-pathogens and a reported yearly increase in gram-positive and decrease in gram-negative-organism-associated SBP may reduce the effectiveness of prophylactic fluoroquinolones and empirical third-generation-cephalosporins. However, SBP-associated-mortality has been reported to decrease, primarily due to prompt diagnosis and treatment. We also found a decreasing trend of mortality, although statistically non-significant. Formulation of guidelines for paracentesis and use of empirical antibiotics and albumin may explain for improved survival. To lower SBP-rates and mortality, there is a need for the continued search for effective prophylaxis with minimal resistance-risk, which may include antibiotic-cycling or non-antibiotic-treatment options.