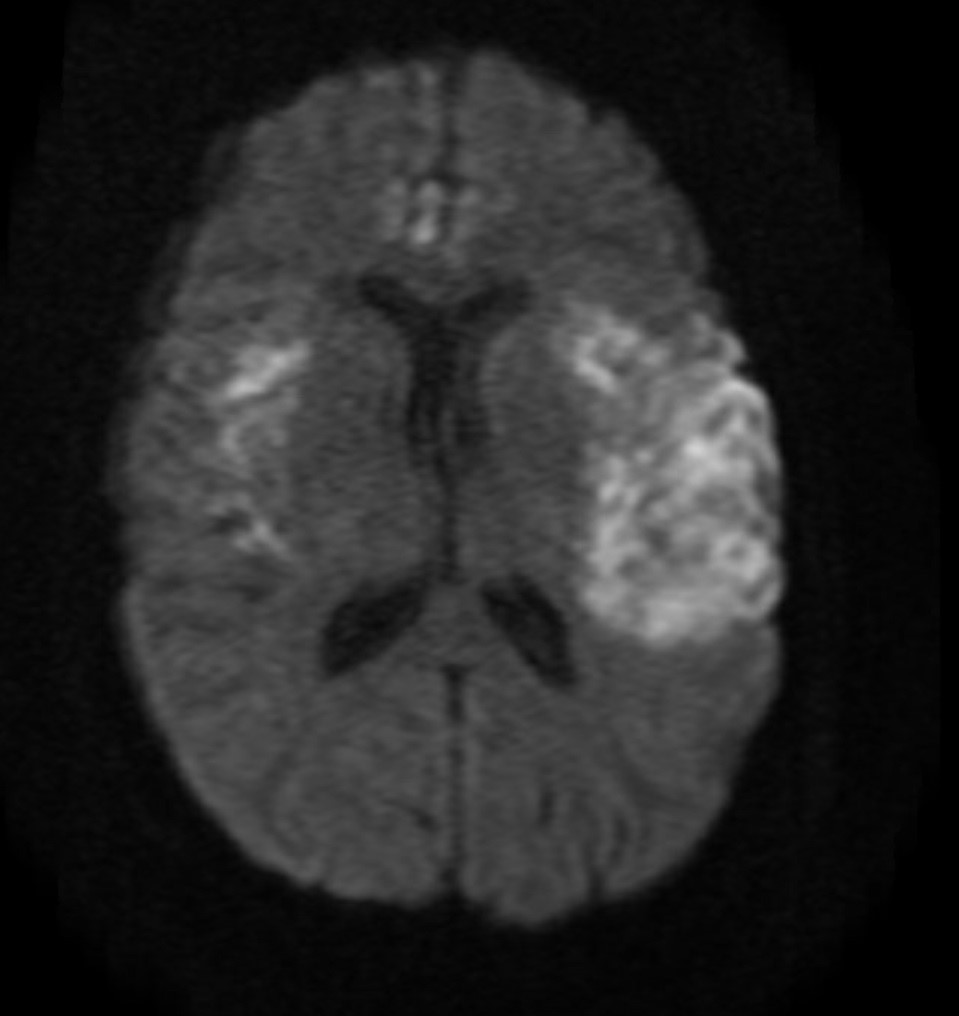
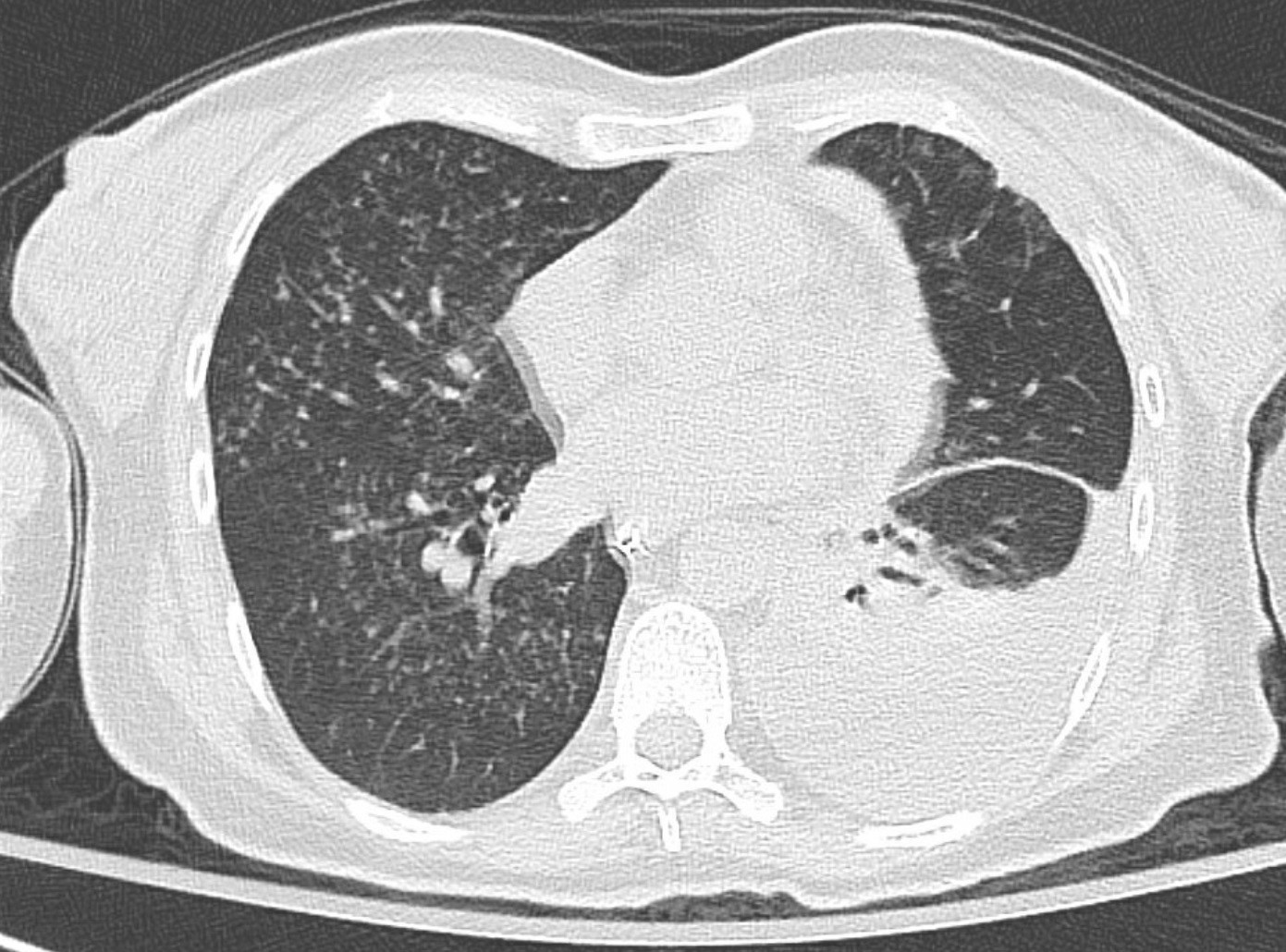
Case Presentation: A 47-year-old female with a history of kidney transplant on immunosuppressive medications presented with worsening confusion and dysarthria for two days. She also reported headache, intermittent fever, and shortness of breath for one month before her presentation. On presentation, her temperature was 103 F, heart rate was 131 b/m, with normal blood pressure and oxygen saturation. Physical exam was remarkable for confusion without focal neurological deficits. Laboratory tests revealed a white blood cell count of 18k/mcl. Brain magnetic resonance imaging and magnetic resonance angiography (MRA) revealed areas of restricted diffusion in the frontoparietal and temporal lobes and bilateral narrowing of the middle cerebral arteries (MCA), (see Figure 1). CT scan of the chest demonstrated left pleural effusion and bilateral pulmonary nodules (see Figure 2). Cerebrospinal fluid (CSF) analysis showed: a total protein of 126 mg/dl, glucose 82 mg/dl, WBC 45 (84% neutrophils), and budding yeast on the fungal stain. Urine and CSF Histoplasma antigen were positive. The patient was started on liposomal amphotericin. Blood and pleural fungal culture grew Histoplasma after two weeks of incubation.
Discussion: CNS vasculitis secondary to histoplasmosis is a very challenging diagnosis giving its variable presentation and its ability to mimic many different pathologies. Our patient presented with finding consistent with CNS vasculitis represented by the MRA finding of bilateral MCA narrowing. The CSF finding of budding yeast and positive Histoplasma antigen led us toward this extremely rare presentation of CNS vasculitis secondary to histoplasmosis and early initiation of antifungal treatment. It is not uncommon for CNS histoplasmosis to be mistakenly diagnosed and mistreated, literature reported cases treated with high dose of steroid early in the course of the disease which led to a rapid worsening of the disease and death in these cases.
Conclusions: Physicians should be vigilant about CNS histoplasmosis as a cause of vasculitis in high-risk patients (immunocompromised and immunocompetent in endemic areas) as early initiation of antifungal and avoiding steroid in the early course favors better outcome.