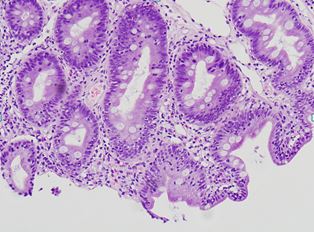
Case Presentation: SH is a 61-year-old male with history of recurrent giardia who presented to the Emergency Department for evaluation of generalized weakness and weight loss in the setting of chronic. Over the past 4 years, he has had recurrent giardia infection despite multiple antiprotozoal agents. Upon presentation, he reported 7 watery, foul-smelling, copious episodes of diarrhea occurring both at night and during the day over the course of a 24 hour period. He denied history of sinusitis, otitis media, pneumonia, bronchitis, meningitis and other medical concerns prior to the onset of diarrhea. He had been undergoing evaluation with Gastroenterology and had no evidence of Celiac disease, Whipple’s disease, amyloidosis, mucosal associated lymphoid tumor, inflammatory bowel disease, partial bowel obstruction or CMV colitis. During his evaluation, he was found to have pancytopenia, acute kidney injury and colitis on CT abdomen and pelvis with IV contrast. Stool pathogen testing revealed positive giardia antigen. HE was treated with IV fluid administration and had resolution of AKI. Tinidazole, albendazole and paromomycin were started for treatment of resistant giardiasis.Further testing revealed pan-hypgammaoglobulinemia (IgA: 7, IgM: 18, IgG 715). He found to have no evidence of acute or chronic pancreatitis, EGD was performed which revealed no evidence mucosal associated lymphoma, Whipple’s disease, Celiac disease, amyloidosis or CMV. Histopathologic slides taken from biopsies of duodenum demonstrated extensive effacement of villi with confirmation of giardia.Vaccine titers were decreased despite being up to date with his immunizations. He was started on treatment for giardia with Tinidazole, albendazole, and paromomycin were initiated for treatment resistant giardiasis. He was discharged with tinidazole, albendazole and paromomycin for treatment of resistant Giardia and outpatient follow-up after receiving vaccinations. Upon follow-up he was found to have persistently decreased vaccine titers and diagnosis of CVID was confirmed.
Discussion: Common variable immunodeficiency is a primary immunodeficiency characterized by impaired immunoglobulin production and/or abnormal B-cells differentiation. It is a clinical disorder that may result from multiple mutations/impaired B-cell differentiation. Commonly, patients present with recurrent infections in adolescents and early adulthood. The typically symptoms of recurrent otitis media, recurrent sinusitis, bronchitis/pneumonia and acute diarrhea. Illnes affects approximately 1 in 25,000.
Conclusions: SH history of recurrent persistent giardia was concerning for immune deficiency. Etiology behind his immunodeficiency cannot be determined as primary immunodeficiency, acquired immunodeficiency(ie HIV), malnutrition induced immunodeficiency(severe protein-calorie malnutrition leading to hypogammaglobinemia) were in consideration. In substantiating a diagnosis of CVID, it is important to obtain vaccine titers and see if there is evidence of adequate titers. If titers are inadequate, vaccination and repeat testing is indicated. If upon, repeat testing there is persistence of low titers a diagnosis of CVID can be made. Prior to testing titers, it is important to see if there is panhypogammaglobulinemia is present and if IVIG has been recently given. Prevention of opportunitistic infection is important as delay in diagnosis leads to increased mobidity and mortality.