Background: Patient-physician communication is essential to medical care. Simple physician behaviors, such as sitting at the bedside, may bolster patient-physician communication.1-3 Yet despite the potential benefit of sitting, prior work suggests that inpatient physicians do not sit frequently.1,4
Methods: Trained staff performed in-person surveys of patients admitted to seven general internal medicine teaching services from August 2019 to January 2020 at an academic hospital. Patients were eligible to participate if they had a length of stay ≥ 2 days, and were excluded if they were unable to provide informed consent, non-English speaking, unable to communicate or visually impaired. We surveyed all internal medicine residents through email via an online platform from November 2019 to January 2020. Here, we report the patient-reported frequency of housestaff sitting at the bedside (primary survey item of interest) as well as the relationship between patient-reported sitting at the bedside and other clinical behaviors, self-reported sitting behavior by housestaff, and housestaff attitudes towards sitting.
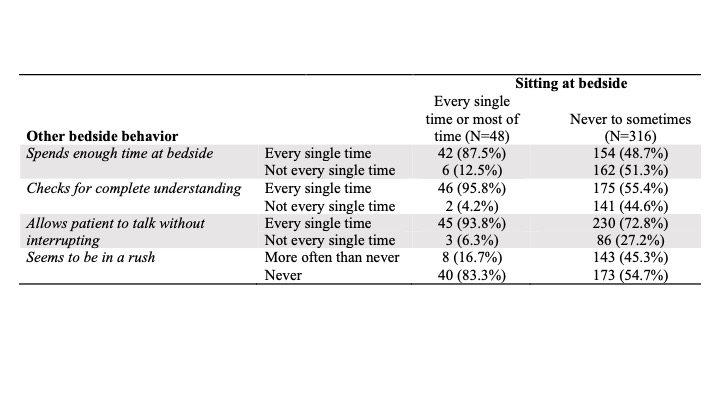
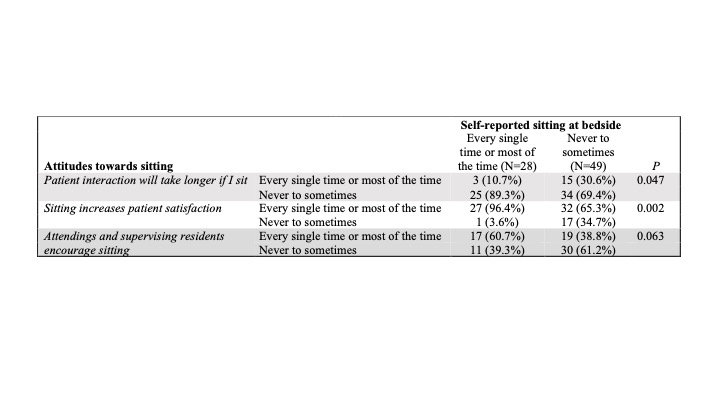
Results: Of 528 screened patients, 334 (63%) were eligible to participate and 256 (48%) completed a survey. Among the 256 patients, 198 (77%) and 166 (65%) reported recognizing the intern and resident on their care team, for a total of 364 completed surveys.Overall, patients reported that the majority of housestaff did not often sit at the bedside: only 13% reported that their identified housestaff sat frequently (most or every single time). In contrast, patients felt that housestaff often engaged in other positive clinical behaviors: 77% frequently spent enough time at bedside, 77% checked for understanding, and 91% did not interrupt. Patients felt that 88% of frequent sitters always spent enough time at bedside vs. 49% of non-frequent sitters (p < 0.01), 96% of frequent sitters always checked for understanding vs. 55% of non-frequent sitters (p <0.01), and 83% of frequent sitters were never in a rush vs. 55% of non-frequent sitters (p= <0.01).Of 151 housestaff, 77 (51%) completed our survey. Twenty-eight (36%) housestaff reported that they sit “every single time” or “most of the time” when interacting with a patient at the bedside. The most commonly cited barrier to sitting was that chairs are not consistently available (38, 45%). 31% of housestaff who reported sitting at the bedside less frequently (e.g., sometimes, rarely, or never) felt that sitting led to longer patient interactions, compared to only 11% of those who reported sitting more frequently (p= 0.047). 96 % of housestaff who reported sitting frequently felt that sitting increases patient satisfaction, compared to only 65% of those who reported sitting less frequently (p=0.002).
Conclusions: Patient-reported sitting at the bedside was associated with patients also reporting positive perceptions of interactions with their physicians, affirming the potential benefit of sitting as an effective communication technique. However, patients reported that housestaff did not frequently sit at the bedside. The discordance between patient and housestaff-reported behavior suggests that physicians may over-estimate how often they sit, although it is also possible that patients may not consistently notice whether a physician sits. Efforts to promote sitting should focus on increasing access to chairs as well as housestaff education given that physician attitudes towards sitting were associated with self-reported behavior.