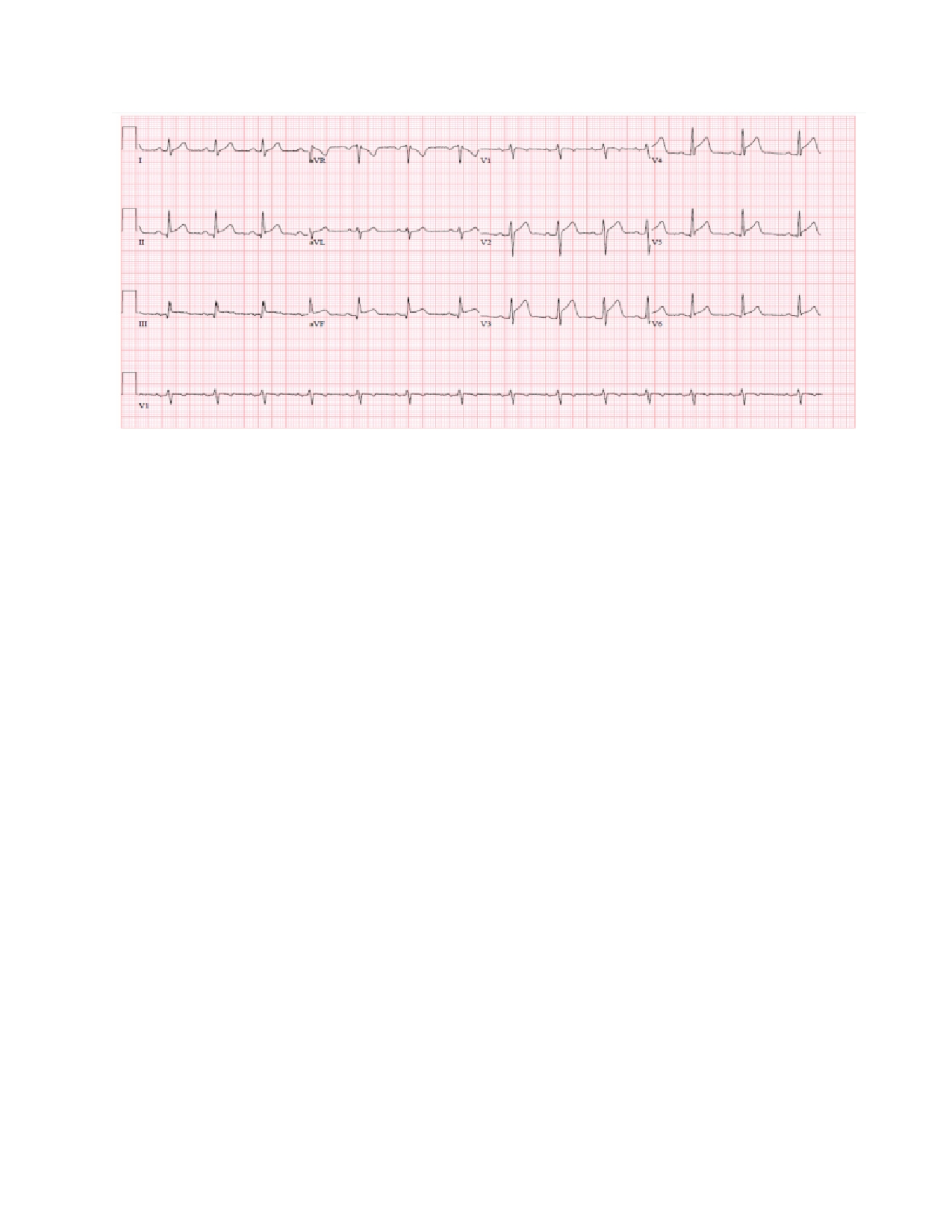
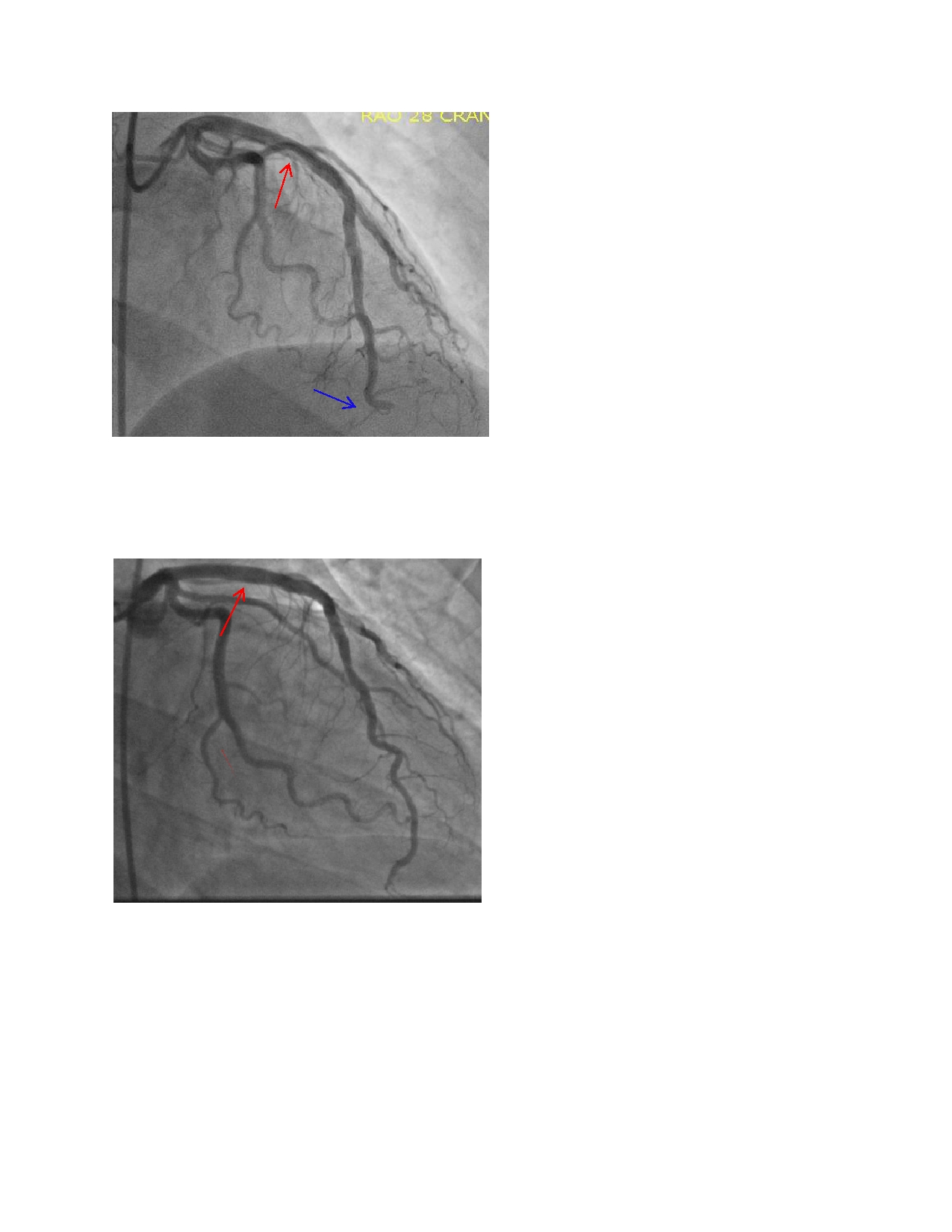
Case Presentation: A 25 year old male with no past medical history was admitted for progressively worsening burning chest pain and shortness of breath associated with diaphoresis, nausea, vomiting, and left arm numbness. Initial electrocardiogram showed STEMI in the inferior and antero-lateral leads, and a troponin of 2.15. Emergent cardiac catheterization revealed a mid left anterior descending (LAD) thrombus with distal LAD embolization. Percutaneous transluminal coronary angioplasty with balloon and thrombectomy restored partial flow to the distal LAD. Eptifibatide, heparin drip, clopidogrel, aspirin, and atorvastatin were started. Repeat angiography three days later revealed persistent large thrombus in the mid LAD with greater than 50% occlusion; therefore, a drug-eluting stent was successfully deployed for recanalization. The patient was continued on dual antiplatelet therapy and rivaroxaban, remained chest pain free with markedly improved symptoms, and discharged home. He was evaluated for hypercoagulable disorders and found to be lupus anticoagulant positive and negative for anti-beta2-glycoprotein I and anticardiolipin antibodies. He was subsequently transitioned from rivaroxaban to warfarin with an international normalized ratio (INR) goal of 2 to 3.
Discussion: Since 2006, the revised Sapporo classification criteria for APS requires detection of at least one of three antiphospholipid antibodies: anti-beta2-glycoprotein I antibody, anticardiolipin antibody, or lupus anticoagulant on two or more occasions at least 12 weeks apart with either arterial or venous thrombosis or an obstetrical morbidity. Lupus anticoagulant correlates strongest with clinical events. While collagen vascular-mediated cardiovascular disease has well defined guidelines and treatment, the optimal treatment for arterial thrombosis in APS is less clear. Depending on expert opinion, treatment is either indefinite warfarin to a target INR of 2 to 3 with or without aspirin, or warfarin alone to a target INR of 3 to 4. Additional recommended treatments and potentially promising therapies including primary angioplasty with stent implantation, direct oral anticoagulant agents (DOACs), heparin, statins, and other novel approaches have been used successfully but remain largely based on case reports and case series.
Conclusions: APS should be considered in young, healthy adult patients who present with classic acute coronary syndrome symptoms without traditional risk factors with an unexplained arterial thrombosis. Treatment is controversial, but most experts recommend warfarin. DOACs do not have any proven benefit or effectiveness for treatment in arterial thrombosis and have a history of recurrent vascular events in the follow-up period.