Case Presentation: An 84 year-old female with metastatic bladder cancer was admitted for a one month history of progressively worsening fatigue, bilateral ptosis, dysphagia, dyspnea, and lower extremity weakness. She was previously diagnosed with localized urothelial carcinoma in 2005 with recurrence in 2017 with pelvic metastases seen on surveillance imaging. She underwent chemotherapy, cystectomy, and hysterectomy with urostomy placement. In late 2018, pembrolizumab was initiated. Two weeks after the first infusion, she was admitted for blurred vision, diplopia, dyspnea, and diagnosed with acetylcholine-receptor Ab-negative myasthenia gravis, secondary to pembrolizumab. She was treated with steroids, pyridostigmine, and IVIG with symptomatic improvement. Three weeks later, she was readmitted with recurrent worsening symptoms requiring emergent intubation for respiratory failure. Solumedrol, pyridostigmine, and IVIG were administered given her prior treatment response. However, due to lack of improvement on the ventilator, plasmapheresis was initiated along with pyridostigmine and prednisone. She received a total of five cycles of plasmapheresis. At the time of discharge, a few months later, she was weaned off her tracheostomy, tolerating oral intake, and on a prednisone taper requiring further rehabilitation at a nursing facility.
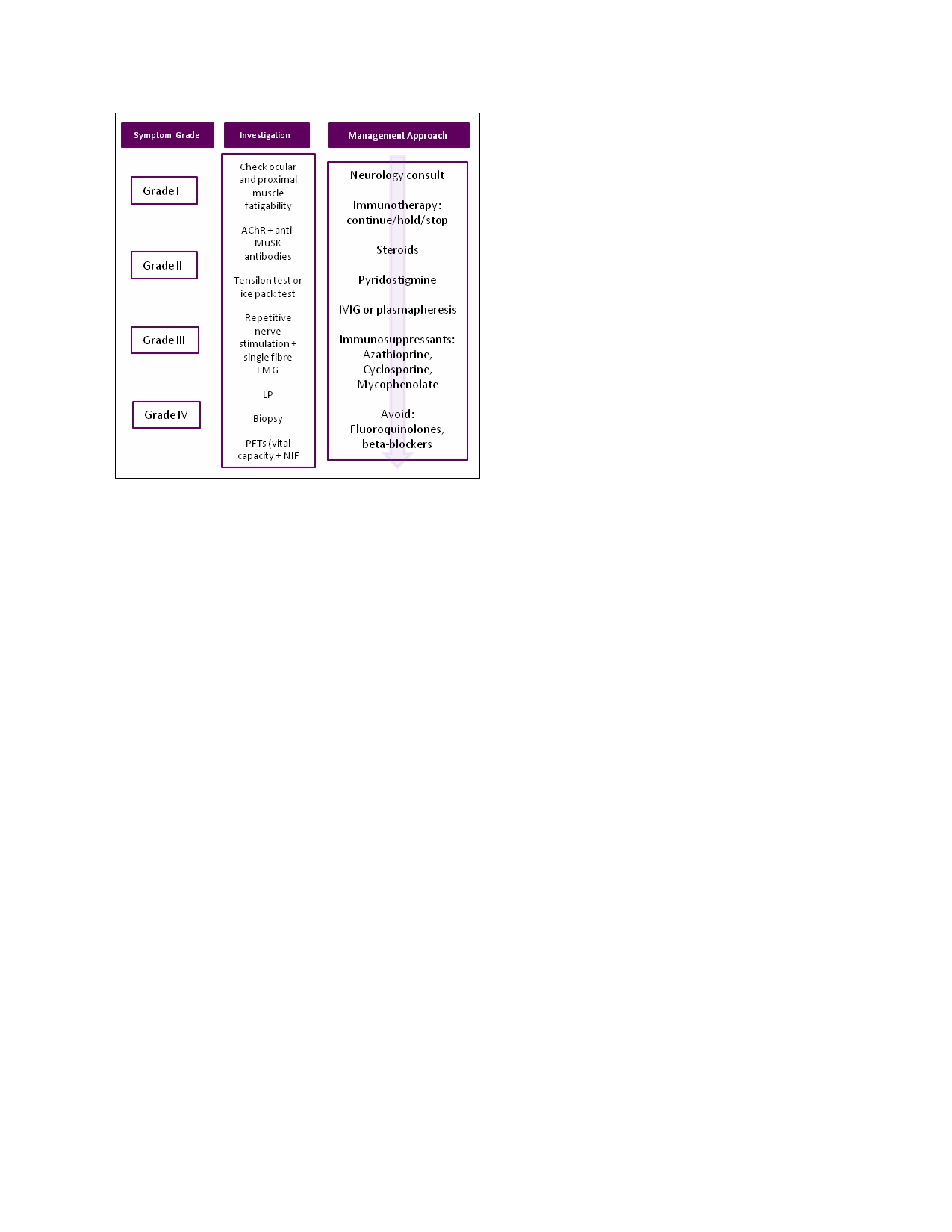
Discussion: Myasthenia gravis should be considered in all patients with malignancies on immunotherapy who present with concerning symptoms. There are only 23 cases of immunotherapy-related myasthenia gravis (irMG) reported in the literature, but this is likely an under-reported complication. Neurological complications can evolve rapidly, usually occurring within 2-12 weeks after initiation, necessitating need for vigilance during all stages of therapy, given ~30% mortality. Diagnosis is based on clinical presentation and supported with positive antibodies, imaging, nerve conduction studies, and lumbar punctures. A grading system is used to characterize severity of irMG to direct therapy, which includes a neurology consult for all grades. Current practice guidelines for grade I include continuing therapy with close monitoring, and grade II include holding therapy, resuming when symptoms revert to grade I or less with consideration of starting corticosteroids. Grades III and IV are treated with holding therapy, initiation of high dose corticosteroids with prednisolone taper for 4-8 weeks, and escalation therapy to IVIG, plasmaphersis, and immunomodulators if needed, respectively. Grade IV toxicities warrant permanent immunotherapy discontinuation.
Conclusions: Immunotherapy has led to promising outcomes over the last nine years accompanied with challenges and limitations due to immune-related adverse events. Prompt diagnosis and rapid therapeutic treatment are the keys to successful management of irMG. In a small subpopulation of patients, some may need extended support to recover.