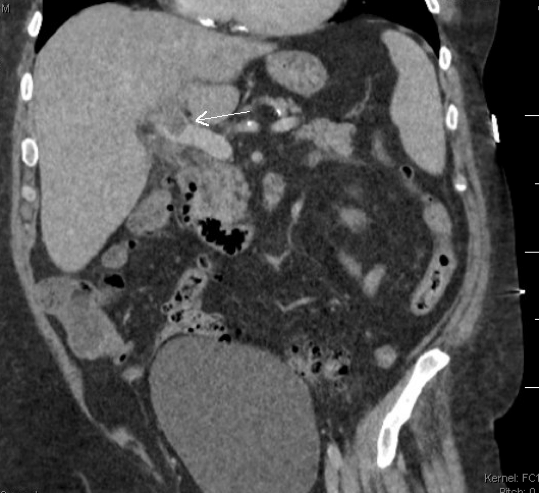
Case Presentation: An 80-year-old man presented with progressive worsening of altered mental status after a fall and right knee trauma. Four days prior he developed subjective fevers, chills and inability to walk after the fall. Past medical history was significant for diverticulitis complicated by diverticular abscess six months prior to admission. He was homebound, no recent travel and no known animal exposures.On physical exam patient appeared acutely ill. Blood pressure was 99/66 mmHg, pulse 104 bpm, temperature 39.5C and respirations 22 bpm. Physical exam was significant for right knee swelling, warmth, erythema and tenderness on palpation. Examination of right knee range of motion was limited by pain. Patient was oriented only to self, no neurological focal deficits present. Hematology was significant for white blood cell count 23 10*3/uL (97% neutrophils). Chemistry showed sodium 127 mmol/L and creatinine 1.810 mg/dL. C-Reactive Protein was 235 mg/dL. Venous blood gas showed lactate 4.79 mmol/L. Computed tomography of head was negative for acute findings. Computed tomography of right knee showed locules of air present within suprapatellar, lateral and medial tibiofemoral joints, no fluid collection identified. Computed tomography with intravenous contrast of abdomen and pelvis was significant for thrombosis of intrahepatic left and main portal vein without signs of hepatic or biliary masses (Figure 1). Blood cultures were collected and urgent right knee arthrocentesis was performed, showing cloudy fluid with 211,800 nucleated cells (97% neutrophils). Patient was started on vancomycin and piperacillin/tazobactam. Synovial fluid culture grew pan susceptible Fusobacterium necrophorum. Blood cultures grew pan sensitive Fusobacterium necrophorum and Clostridium clostridioforme. Prior antibiotics were discontinued and patient was switched to cefepime and metronidazole. His mental status and right knee symptoms improved. He was discharged on an eight-week course of metronidazole for anaerobic polymicrobial bacteremia.
Discussion: Fusobacterium necrophorum is an anaerobic gram-negative rod residing as normal flora in oral and gastrointestinal tracts. Infection typically presents as sore throat and can cause peritonsillar abscess to bacteremia. André Lemierre was the first to describe a syndrome with septic thrombophlebitis of the internal jugular vein causing metastatic infections including septic arthritis. Reports of Fusobacterium necrophorum leading to joint infection and bacteremia have been detailed in young adults with a history of recent dental surgery. To our knowledge, this is the first case of disseminated Fusobacterium necrophorum presenting in an elderly patient.Prior literature has described a gastrointestinal variant of Lemierre syndrome, in which hematogenous spread occurs through portal circulation in the setting of diverticular disease or intra-abdominal abscess. Of note, computed tomography of abdomen and pelvis with intravenous contrast done six months prior to admission in our patient did not show signs of venous thrombosis. Underlying malignancy should be excluded in patients with Fusobacterium necrophorum bacteremia and non-head primary foci, with outpatient screening colonoscopy.
Conclusions: Lemierre’s syndrome typically presents as oral infection complicated by septic thrombophlebitis of the internal jugular vein. We describe a rare case of a gastrointestinal variant from possible diverticular spread leading to polymicrobial bacteremia.