Background: Uncertainty of viral transmission and PPE availability early in the SARS-CoV-2 pandemic created unique infection control challenges for hospitals. Prior to masking recommendations and widespread testing availability, the hospital medicine service at an academic hospital system published “medical distancing” guidelines to reduce the frequency and proximity of physician-patient interactions to minimize transmission. While previous studies suggest that isolation precautions lead to patient perception of decreased care coordination, increased adverse events, and overall decreased satisfaction with care, the impact of medically distant care on patient experience during a pandemic is not well characterized (1-4).
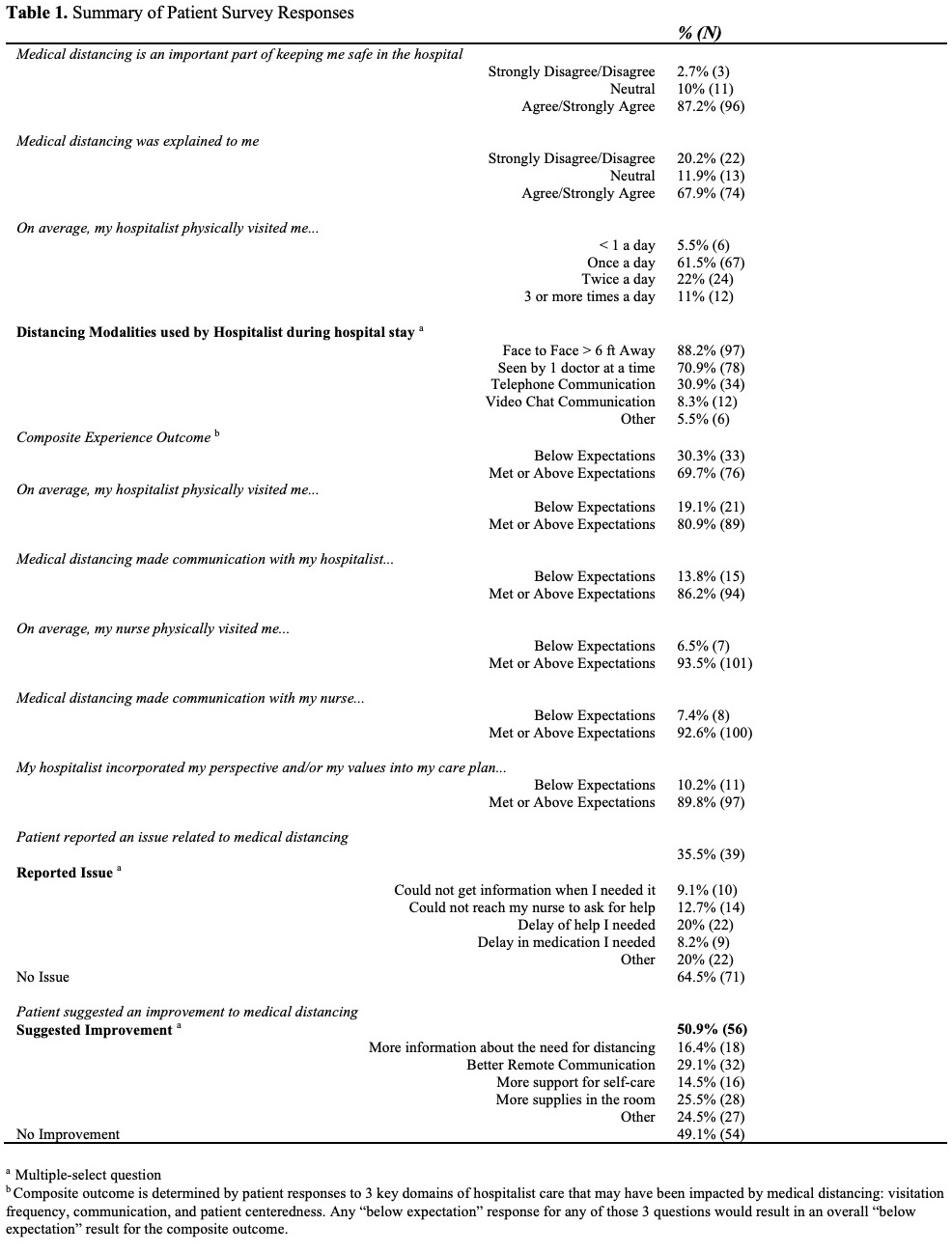
Methods: A 12- item questionnaire was administered by phone to English or Spanish-speaking adult patients discharged from the Hospital Medicine service from 3/15/2020 – 8/15/2020. Questions attempted to measure patient perceptions of how medical distancing impacted communication, care quality, timeliness of care, and patient-centeredness during their hospital stay. Most responses were recorded using a 5-point Likert scale. Descriptive statistics and 2-sided χ2 analyses were used to characterize the study sample and test statistical significance.
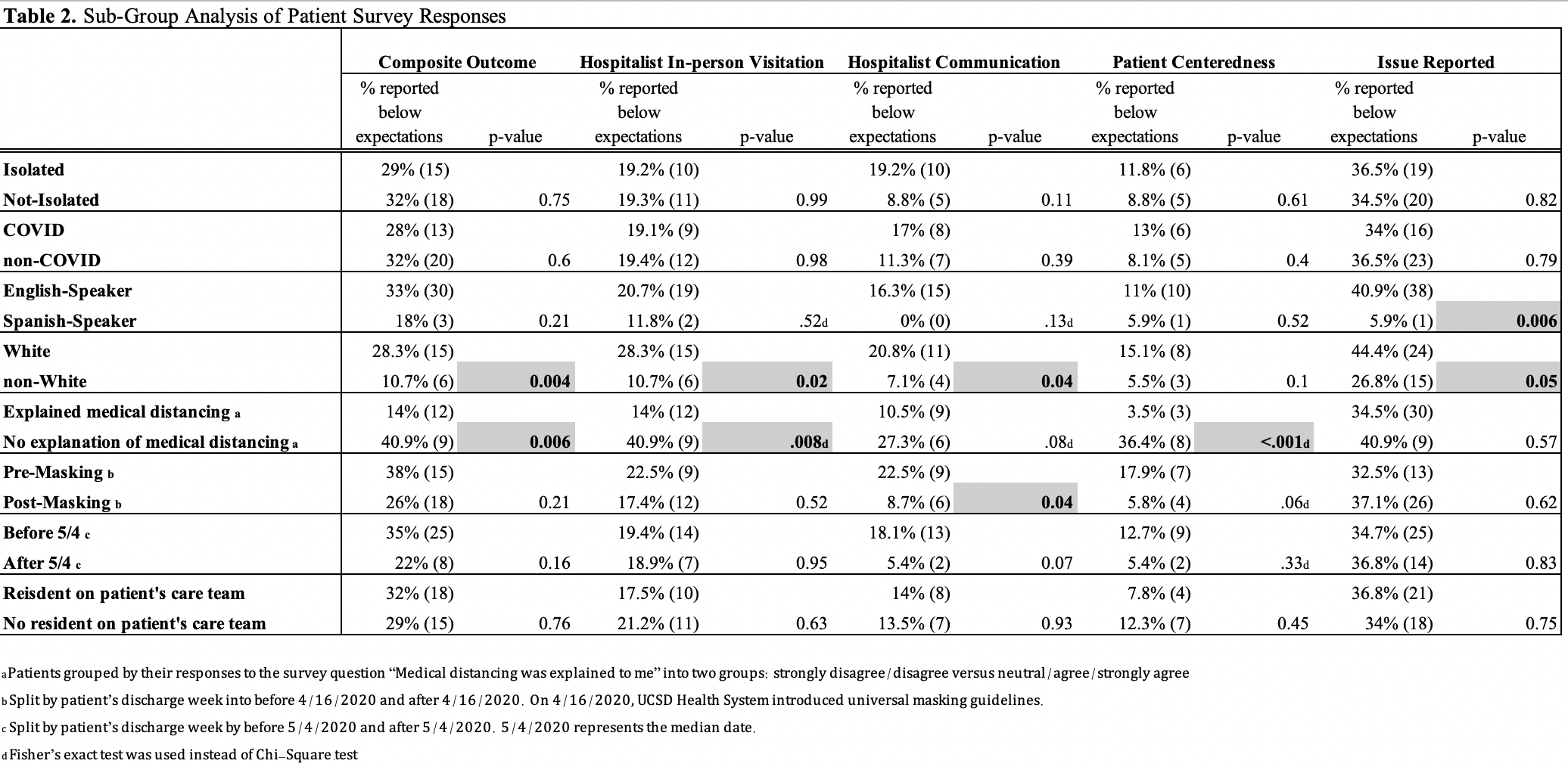
Results: 110 patients consented to and completed the survey. Surveyed patients identified as 49.1% White, 34.5% Hispanic, and 8.2% Black. 42.7% of patients had known or suspected COVID-19 infection. 47.3% were isolated, with a mean of 3.57 isolation days. 87.2% of patients agreed that medical distancing was important for keeping them safe. 30% of patients reported below-expectation care for any of the three hospitalist experience domains: visitation frequency, communication, and patient centeredness (measured as the composite experience outcome). There were no significant differences in measured experience domains for patients with/without COVID-19 diagnoses, or isolated/non-isolated patients. Both patients who identified as White (versus non-White) and those who did not recall receiving an explanation for medical distancing (versus those who did recall an explanation) were more likely to report below-expectation care in the composite experience outcome (p = 0.004 and 0.006, respectively). A significant difference between hospitalist communication before and after implementation of a universal masking mandate was found, where 22.5% of those surveyed rated negative hospitalist communication before implementation compared to 8.5% after (p = 0.04). Results showed a similar trend toward negative perceptions of communication earlier in the pandemic (pre vs post-median date of discharge (p = 0.07)).
Conclusions: Most of the patients surveyed were satisfied with their care experience despite medical distancing. Isolation status did not affect patient experience. However, non-White race, recall of an explanation for medical distancing during hospital stay, and discharge date after the implementation of a universal masking mandate were all associated with better self-reported patient experience. This study was single center and retrospective, limited by the relatively small number of patients reporting negative experiences and recall bias of patients who participated. This study was the first of its kind to characterize patient perceptions of care in relation to demographic and clinical differences during the early part of the COVID-19 pandemic.