Background:
Although it is important for physicians to be involved with initiatives to enhance patient safety, little training is devoted to this area. In addition, the topic is challenging to teach, as house staff may prefer discussing specific conditions rather than quality improvement.
Methods:
We developed a longitudinal curriculum to teach the key aspects of patient safety in an interactive manner that progresses over the 3 years of residency. There are 5 primary components. First is the interactive core lecture (level — intern; venue — ambulatory block; key concepts introduced — the nature, prevalence, and categories of medical errors, tools used to improve quality). The plan‐do‐study‐act (PDSA} cycle is modeled. House staff members are divided into groups and presented with a case (e.g., hypoglycemia from inadequate medication reconciliation) and assisted in developing a PDSA cycle. Second is reflective exercise on discharge summary quality (level — intern; venue — medicine ward rotation; each intern self‐scores 1 of his or her discharge summaries using a standardized tool and the medical record as the reference). The evaluation is reviewed with an attending, and deficiencies are discussed. Third is hospital hazards (level — PGY1‐3; venue — attending rounds, 1/month; resident teams independently evaluate a patient's room for hazards, for example, call bell out of reach). Teams reconvene to discuss their findings. Fourth is the mini‐root cause analysis (mini‐RCA) [level — presenter‐PGY3; participants — PGY 1‐3; venue — house staff quality improvement conference (QIC), 1/month; a PGY3 leads a mini‐RCA, which focuses on an actual error from the teaching service]. Prior to the conference, the resident is responsible for investigating the error, including speaking with involved staff. The case is presented, the “root causes” are identified, and potential solutions are discussed by the house staff in attendance. An introductory segment to the QIC introduces advanced concepts, including RCAs and the regulatory environment for hospital improvement (Joint Commission, CMS). The fifth primary component is resident quality projects (level — PGY 2‐3; venue — optional resident activity; the Department of Medicine provides a $2500 grant for interested residents to perform a mentored scholarly project related to hospital quality). To date, 18 residents have performed projects.
Results:
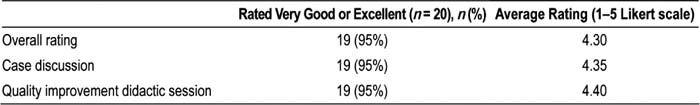
A survey is distributed after each QIC, and evaluations are being collected on all aspects of the curriculum. Data from the first 2 months' experience of the QIC are presented in Table 1. Evaluations indicate that the curriculum has been well received by house staff. Other main findings were: 90% agreed that their “knowledge of issues related to hospital quality has been enhanced by this conference”, and 90% agreed that “solutions discussed at this conference could lead to improved patient care”.
Conclusions:
Our longitudinal curriculum engages learners to provide the knowledge base and skills to enable them to participate and eventually lead initiatives focusing on improving hospital quality.
Author Disclosure:
A. Dunn, none; J. Goldenberg, none; N. Kathuria, none; K. Smith, none; M. Pourdehnad, none; J. Nissim, none; B. Markoff, none; R. Jervis, none; L. Peccoralo, none; J. Litrivas, none.