Background: Early diagnosis and treatment of sepsis improves patient outcomes. Diagnosis requires an objective component (currently at least two Systemic Inflammatory Response Criteria, SIRS) and a subjective, clinical suspicion of infection. While much attention has been placed recently on the ideal objective criteria to accurately identify sepsis, little is known about the agreement among providers with regards to subjective assessments and the impact of that agreement on patient outcomes.
Methods: We conducted a secondary analysis of prospectively collected data that included all consecutive adult patients hospitalized on a general medicine ward from 4/1/14 to 4/1/15. Bedside nurses (RN) documented their suspicion of infection using a paper-based screening tool every 12 hours. This was compared to the physician or advanced practice professional (MD/APP) suspicion – defined as an existing order for antibiotics or a new order for blood or urine cultures in the 12 hours prior to the nursing screen time. The primary outcome was progression to severe sepsis or septic shock. Concordance rates were assessed using a kappa statistic. A chi-squared test and non-parametric test for trend were used to evaluate for differences in outcomes based on provider agreement.
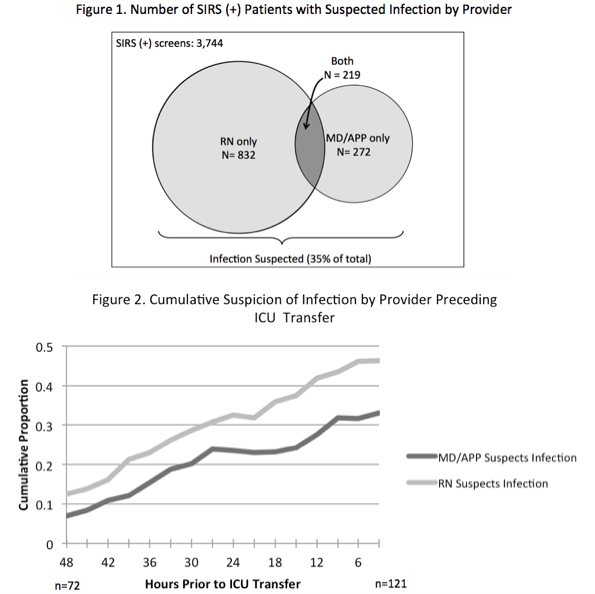
Results: During the study period, 1,386 distinct patients yielded 11,489 screens. Of those, 3,744 (32.6%) met SIRS criteria, in which suspicion of infection was noted by both the RN and MD/APP in 5.8%, RN only in 22.2%, MD/APP only in 7.2%, and neither in 64.7% (Figure 1). This resulted in an agreement of 17.2% for the presence of infection (κ= 0.12, p<0.001). Progression to severe sepsis or shock was significantly higher when both providers suspected infection in a SIRS positive patient (17.7%) and lowest when neither suspected infection (1.5%), with single-provider suspicion associated with intermediate risk (6.0%), p<0.001. For patients transferred to the ICU, RNs were more likely to suspect infection at all time points compared to MD/APPs (Figure 2). The difference was small 48 hours preceding ICU transfer (12.5% vs 6.9%, p=0.40) and became more pronounced by 3 hours prior (46.3% vs 33.1%, p<0.05).
Conclusions: Discordance between provider suspicion of infection is common, with RNs documenting suspicion earlier and more frequently than MD/APPs. Suspicion by either provider alone is associated with a moderate risk of sepsis progression. Thus, a collaborative method that includes both RNs and MD/APPs may improve the accuracy and timing of sepsis detection on the wards.