Background:
Diagnostic MR imaging of osteomyelitis in the hospital setting continues to guide patient care and treatment when plain films are inconclusive. However, even MRI with gadolinium can be non-specific in patients with other forms of sterile inflammation, leading to overtreatment in the form of invasive procedures and lengthy antibiotic regimens. Ferumoxytol is an iron oxide nanoparticle formulation that specifically localizes to areas of active inflammation after intravenous injection: the iron oxide is taken up by macrophages from the bloodstream as they hone in on areas of infection, and altered magnetic field is observed as negative enhancement on T2-weighted sequences. Our objectives were (1) to show that ferumoxytol causes negative enhancement on T2-weighted MRI sequences in cases of histologically proven osteomyelitis and (2) to compare these findings to the interpretation of baseline gadolinium MRIs by blinded radiologists.
Methods:
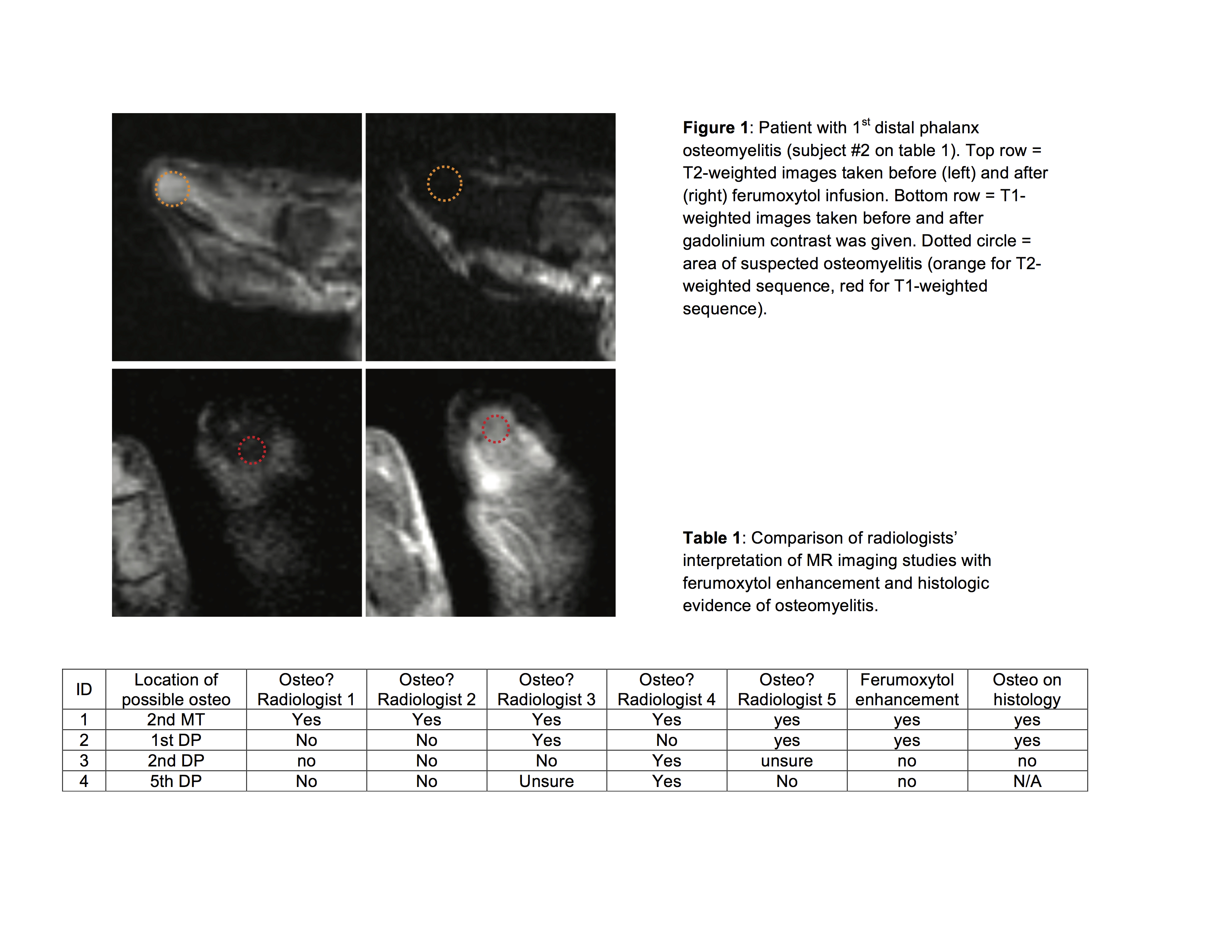
The study was approved by the IRB. Patients admitted with suspected osteomyelitis were identified by chart review. Those who required an MRI for suspected osteomyelitis were approached for informed consent to participate in this study, which involved another MRI 12 to 26 hours after ferumoxytol infusion. Tissue sections were gathered from patients who later needed amputations; these were interpreted by faculty in pathology. A panel of 5 blinded radiologists independently reviewed the baseline non-ferumoxytol MRIs for presence or absence of osteomyelitis using standardized criteria. Pixel analysis was performed on ferumoxytol MRIs to quantify significant changes in contrast between regions of interest within slices and between sequences.
Results:
Four patients were enrolled in this initial pilot study, each with a soft tissue wound in the lower extremity. Two patients had histology-proven osteomyelitis, with a significant negative enhancement from ferumoxytol over the infected area on T2-weighted imaging. A third patient’s tissue sample was negative for osteomyelitis and his ferumoxytol MRI did not negatively enhance in the negative direction. The final patient did not have tissue available for histology – in this case, gadolinium significantly enhanced while ferumoxytol did not. Only one out of four patients was given the diagnosis of osteomyelitis by all five independently reading radiologists.
Conclusions:
Ferumoxytol causes significant T2-weighted negative enhancement in areas of histology-proven osteomyelitis, but not in areas without osteomyelitis. Ferumoxytol enhancement, gadolinium enhancement, and radiologists’ reads are often discordant. Based on the accuracy of ferumoxytol enhancement in this study, it is possible that incorporating ferumoxytol enhancement into the diagnostic algorithm for osteomyelitis on MRI will also allow for greater diagnostic precision by reducing the variability of image interpretation between radiologists.