Background:
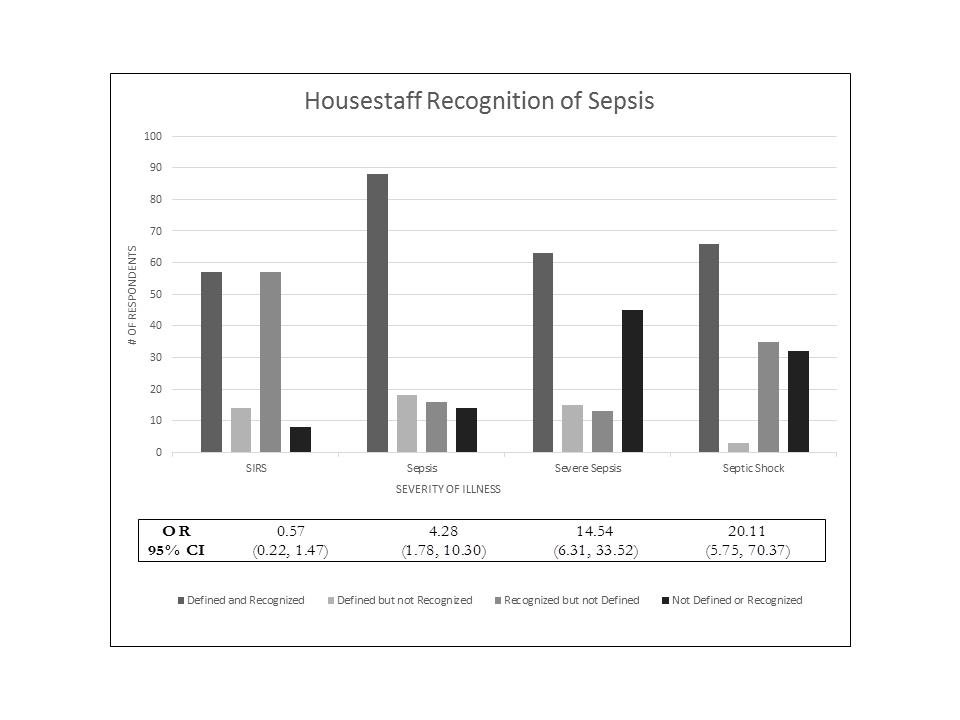
Severe sepsis is the number one cause of hospital mortality. Despite decades of bench and clinical research on sepsis, the only intervention that consistently decreases mortality is early recognition of the disease and antibiotic administration. We surveyed 136 house officers and 280 nurses and found that they were able to recognize sepsis in clinical vignette form 56% and 17% of the time, respectively. With this knowledge, we felt we needed to leverage the power of the EMR to build a sophisticated, two-tier, Modified Early Warning System (MEWS) with accompanying best practice alerts (BPAs) and order sets to help providers recognize sepsis and initiate therapy in a timely manner, as specified in the Surviving Sepsis guidelines.
Purpose:
To recognize decompensating patients early and, if septic, to initiate surviving sepsis 3 hour bundled care.
Description:
Within the EPIC EMR we built technology that calculates a MEWS score in real time. This MEWS score is then able to be displayed on any patient list view in EPIC. If a nurse or nursing assistant enters in only one vital sign, and that vital sign is abnormal, a BPA will then prompt the nursing staff to enter a full set of vital signs. With the full set entered the MEWS is calculated and if it exceeds a predetermined first tier threshold, EPIC pages the unit charge nurse and the primary team. When the bedside nurse then opens the patient’s chart he/she is directed to an order set that orders a stat and a 4 hour repeat lactic acid level, blood cultures, and increased frequency of vital signs. When the provider enters the chart, and if infection is likely, they are directed to an order set where they choose a site of infection and enter labs and antibiotics predetermined by the infectious disease department. If the MEWS exceeds the second tier threshold, the charge nurse and a rapid response team is paged to evaluate the patient, draw point of care labs and evaluate for transfer to a higher level of care.
Conclusions:
Eight weeks into our pilot on one acute internal medicine unit, we have found the system to be successful. Of 12 alerts; 11 patients had sepsis and 9 of those had severe sepsis. We have had one second tier alert which triggered a rapid response. This patient was found to have hospital acquired severe sepsis and, as a result of our protocol, a lactic acid and blood cultures were drawn within 30 minutes and antibiotics were initiated within one hour. Ten hours later, those blood cultures became positive with b- hemolytic Streptococci.Our system has shown to successfully alert providers to unstable patients, and has helped those patients receive treatment more quickly. Over the coming months, the system will be disseminated to other units.