Background: Many academic hospital medicine programs have reached a critical transition point as they attempt to sustain and develop growth in their non-clinical, academic missions. To meet increasing clinical needs, the Duke Hospital Medicine Program (DHM) has grown rapidly to over 100 providers dedicated to careers in academic hospital medicine. The majority of this group has been in practice for less than ten years. This rapid growth and relative youth parallels that of many other programs. This may contribute to burnout, difficulty in retention, and a lack of engagement in the non-clinical missions among academic hospitalists. Given these concerns, we sought to evaluate the academic interests and needs of our large faculty and, subsequently, inform our growth in resources and funding that support our hospitalists’ academic careers.
Methods: We surveyed of 80 hospitalists between October and November 2017 at DHM’s two clinical sites, a 957 bed tertiary care center and a 369 bed community hospital. All hospitalists received a 27 item, anonymous survey followed by three reminders for survey completion. We surveyed participants about factors that led to their choice of career, their areas of academic interest, additional resources or skills needed to sustain or grow their academic productivity, and how they gauged success in the field of hospital medicine. Additionally, we sought to assess their current degree of professional burnout.
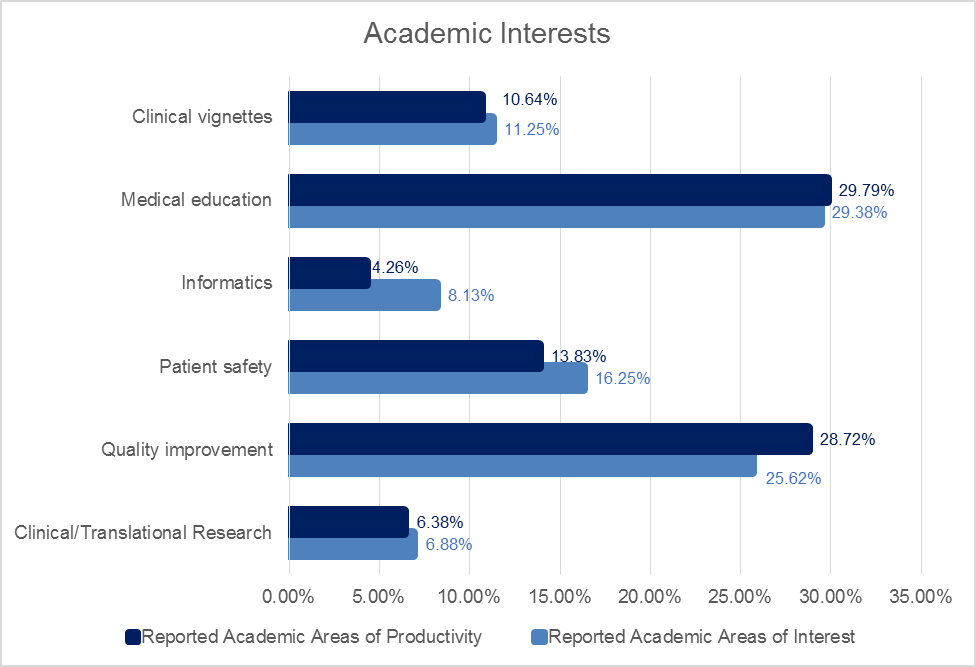
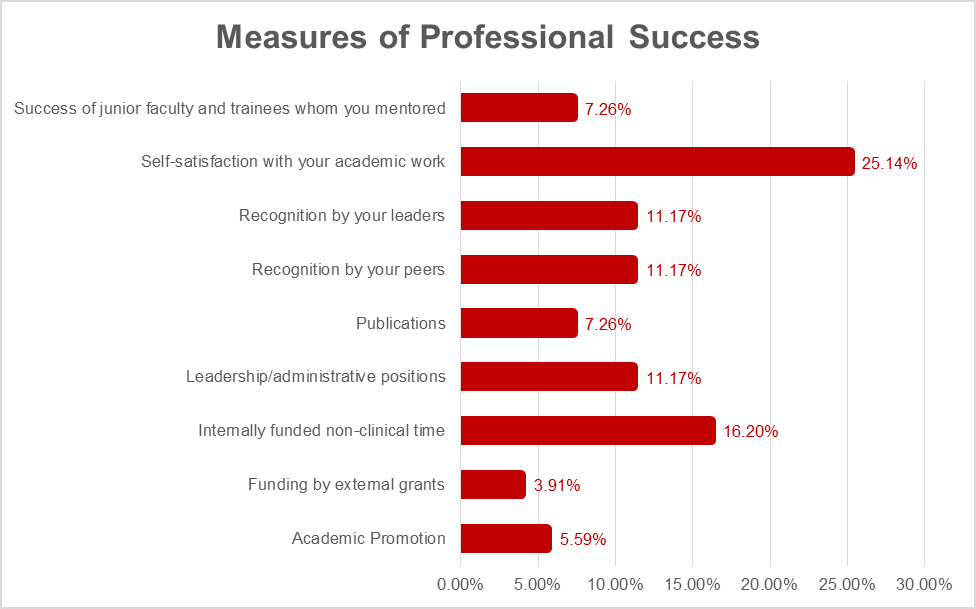
Results: Survey response rate was 76.2%. DHM’s physicians reported choosing their career for the academic environment of practice (22.4%), a desire to teach learners (22.4%), and exposure to complex illnesses (10.28%). Less than 10% of respondents reported access to mentorship, institutional values in quality improvement, or a desire to do research were within their top three reasons to choose their career. Nonetheless, a majority of respondents reported some degree of academic productivity within an area of interest (82.2%), predominantly medical education (30.8%) or quality improvement (29.8%). A majority of clinicians were interested in becoming further engaged in academic projects (69.3%). Protected non-clinical time (26.5%), formation of teams to share workloads (18.4%), and additional training opportunities (14.3%) were the top needs identified to improve academic engagement. Self-satisfaction with academic work (25.1%) and earning internally funded protected time (16.2%) were the top reported indicators of career success in hospital medicine. At the time of this survey, 40.3% of respondents reported some degree of burnout.
Conclusions: This survey provides a unique opportunity to evaluate the baseline engagement of a large academic hospital medicine group. The majority of DHM’s faculty wants to engage in the non-clinical, academic missions, including education, quality improvement, and research. However, publication and acquisition of external grant funding are not the largest drivers of this interest. Rather, faculty report more interest in garnering internal funding for protected time and increasing their self-satisfaction with their academic work. Our survey findings present important insights into the attitudes, needs, and motivators for hospitalists interested in engaging in academic projects. As programs continue to balance efforts to meet clinical demands, cultivate the academic interests of faculty, and develop track records of academic productivity, these findings may have broader implications to other academic programs.