Background: Chronic Obstructive Pulmonary Disease (COPD) is the third leading cause of hospital readmissions in America. Over one-third of patients admitted for COPD exacerbations are readmitted within 90 days, with readmissions costing $15 billion. Medicare instituted financial penalties for excessive readmissions after COPD hospitalizations, incentivizing the creation of readmission prediction tools. Two such tools, the general HOSPITAL score and COPD-specific PEARL score, rely on variables that may be unlikely to be available for use in real-time. We aimed to develop a COPD-specific model using real-time electronic health record (EHR) data to predict 90-day readmissions before patient discharge.
Methods: aAll adult patients admitted at a large urban medical center between November 2008 and June 2016 were eligible for inclusion if they had a primary or secondary ICD-9-CM diagnosis code of COPD or if they were treated for a COPD exacerbation. Patient demographics and encounter-level data including vital signs, laboratory values, and medications administered were retrieved from the EHR for these patients. This cohort was then split randomly into a derivation set (60%) and a validation set (40%). The derivation set was used to train a random forest machine learning model (RFML), while the validation set was used exclusively to assess RFML performance via the area under the receiver operating characteristic curve (AUC) statistic.
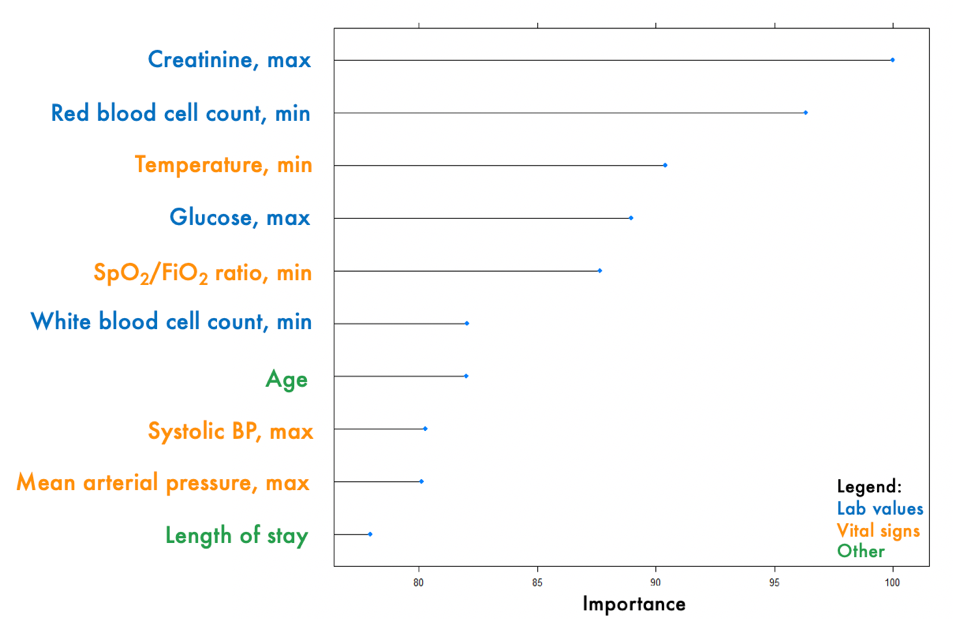
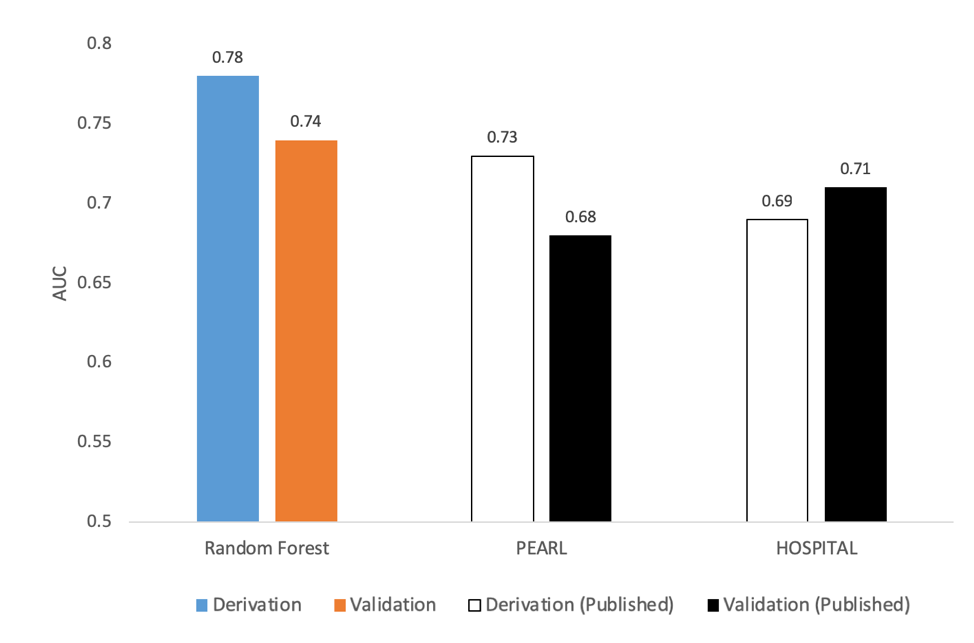
Results: Of the 182,940 admissions during the study period, 1,328 met our inclusion criteria, of which 306 had a 90-day readmission. The most important predictors for 90-day readmission included maximum creatinine value during the encounter, minimum red blood cell count, and minimum body temperature (Figure 1). Other predictors included the results of respiratory cultures and whether the patient was admitted during the winter months. At the 90-day prediction horizon, RFML had an AUC of 0.78 in the derivation set and an AUC of 0.74 in the validation set. This compares favorably to the HOSPITAL and PEARL scores, which have published validation AUCs of 0.71 and 0.68, respectively (Figure 2).
Conclusions: Our model for 90-day readmission prediction shows potential for improved predictive performance over the HOSPITAL and PEARL scores. Future work should compare our model to the published algorithms using the same dataset. However, since our score exclusively uses EHR data, it could be integrated into EHRs for real-time readmission risk prediction. This would help physicians provide personalized treatment focused on reducing COPD readmission, improving quality of care, and reducing medical expenditures.