Background: ED visits increased to 145.59 million in 2016 (CDC 2019), resulting in an increase in hospital admissions. Chen et al. showed a correlation between the overall ED census and likelihood of admission; while, Velasquez et al. found up to 28% of hospitalists reported having admitted patients when no admission criteria were met. They described the role of the hospital medicine triagist as a physician who fields admissions requests and navigates appropriate disposition. We performed a cost-benefit analysis to determine the value of our triagist program.
Methods: We took the organizational perspective in performing the cost benefit analysis. Our hospital medicine triagist program consists of one hospitalist performing triage duties day (0700-1500), evening (1500-2200) and night (2200-0700). We calculated the gross annual cost of the program to include 2.0 FTE each for day and evening shift (182 annual shifts/FTE), and 2.3 FTE for the night shift (156 annual shifts/FTE). Average annual compensation/FTE is $230,000 + 20% benefit rate = $276,000. Net annual cost was calculated by multiplying gross annual cost by proportion of clinical productivity lost. Proportion of triagist clinical productivity was calculated by dividing mean total visits/24hrs of the 3 triagists by 18 visits/24hrs – the typical productivity of 3 admitters.We calculated the benefits of our triagist program to include hospital bed days saved and staffing saved for decreased census. For every called admission that was prevented, we attributed one hospital day in cost savings. At our hospital, a non-telemetry floor bed costs $700/day (charge of $2500/day) with an average reimbursement of $375/day for a net cost of $325/day. We calculated the decreased staffing needed for a smaller census by dividing census days saved by 14 (typical census of our rounding physicians). This fraction was multiplied by 2.0 FTE/rounder and then by $276,000/FTE to determine a net annual staffing cost savings.Data kept on the triagist spreadsheet from July 1, 2019 – October 31, 2019 was analyzed for (1) the number of calls fielded, (2) number of visits performed/shift and (3) number of admission requests discharged to home.We performed a sensitivity analysis to determine the breakeven point for our triagist program.
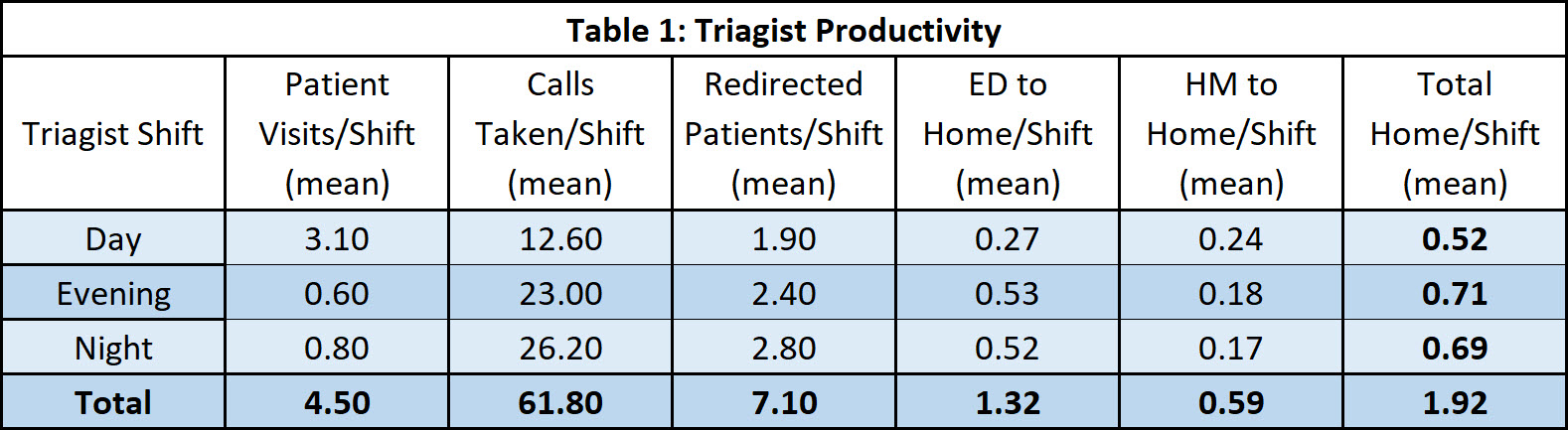
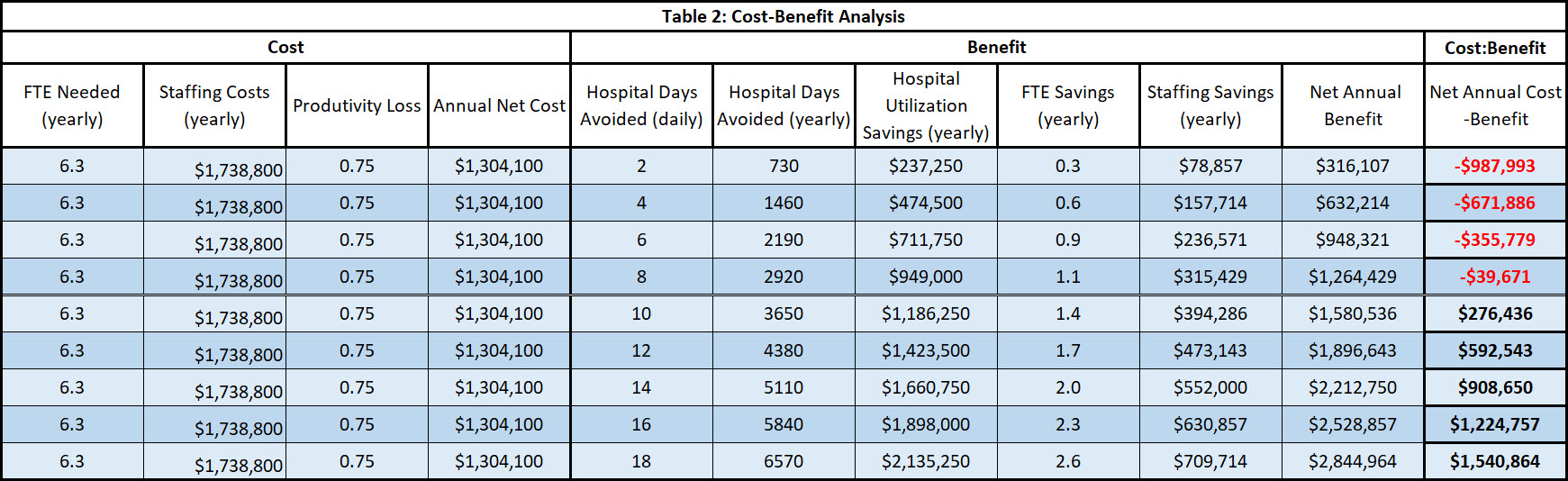
Results: On average, our triagists field 61.8 calls, perform 4.5 visits and avert 1.92 admissions daily (Table 1).CostsGross annual program cost: 6.3 FTE/year * $276,000/FTE/year = $1,738,800Triagist clinical productivity: 4.5 visits/24 hrs / 18 visits/24 hrs = 0.25 (75% lost clinical productivity)Net Annual Program Cost: 0.75* $1,738,800 = $1,304,100BenefitsHospital Utilization Benefits: 1.92 admissions avoided * 1 day aLOS = 1.92 bed days saved/24hrs * $325/bed day = $624 saved/day * 365 days/year = $227,760 in bed day costs saved/yearFTE Savings Benefits: 1.92 admissions avoided * 1 day aLOS = 1.92 patient days saved/24hrs 1.92 patient days / 14 patients/rounder = 0.137 rounders saved * 2.0 FTE/rounder = 0.274 FTE saved/year * $276,000/FTE/year = $75,703 in FTE cost savings/yearNet Annual Program Benefit: $227,760 + $75,703 = $303,463Net Annual Cost-Benefit: $303,463 – $1,304,100 = <$1,000,637> (Table 2)
Conclusions: By averting 1.92 admissions daily (3.1% of calls fielded) our triagist program results in an annual organizational loss of $1,000,637. To break even, our triagists need to avert 8.25 admissions/day. Other benefits of the triagist program may include increased productivity of other admitters and improving utilization of other services.