Background: Sepsis is a leading cause of hospital death and readmission (1-2). Prior work has suggested that early, adequate intravenous fluid (IVF) administration during sepsis care is associated with lower mortality, even among those at risk for fluid overload (including patients with chronic kidney disease [CKD] or heart failure [HF]) (3). At the same time, emerging evidence suggests that excess fluid accumulation may be harmful (4-10), with many concerned about positive fluid balance in sepsis contributing to adverse post-sepsis sequelae. Understanding the impact of fluid balance on sepsis readmission could offer a tangible approach to reducing adverse outcomes. However, a critical gap exists in understanding fluid practice for sepsis outside of the intensive care unit (ICU). While Tang et al showed that nearly 80% of sepsis patients do not require ICU care (11), there is little evidence available to guide practice.We therefore undertook this study to evaluate whether positive fluid balance among non-critically ill sepsis patients was associated with readmission, including readmission for HF.
Methods: We conducted a retrospective cohort study of adult sepsis patients from 2012-2017 in an integrated health system. We identified patients admitted through the emergency department who met Sepsis-3 criteria within 6 hours of presentation. We excluded patients who spent any time in the ICU, died during hospitalization, had length of stay (LOS) > 7 days, end-stage renal disease, acute liver failure, or hypoalbuminemia. Our exposure of interest was net fluid balance (I/O), measured at daily intervals and characterized as positive vs negative at discharge. Our primary outcome was 30-day all-cause readmission. Our secondary outcomes were 30-day readmission by category (HF, infection, other) and mortality after living discharge. We used multivariable competing risk survival analysis (12-13) and Kaplan Meier survival analysis.
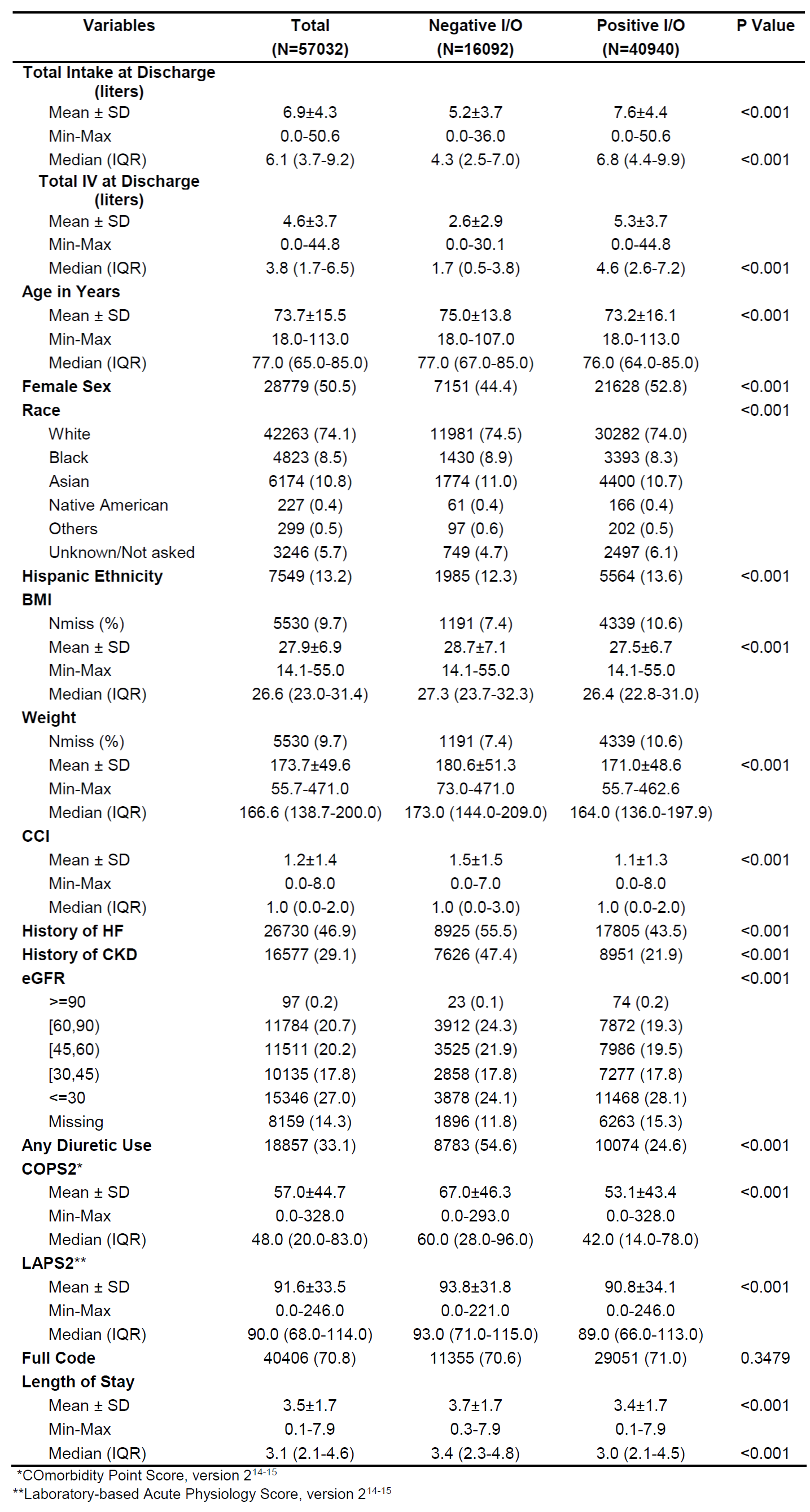
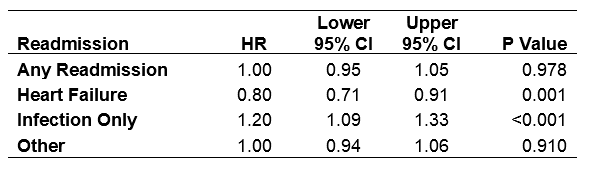
Results: Our study included 57,032 sepsis patients admitted to a non-ICU setting who survived to discharge. Table 1 describes baseline characteristics comparing negative (28.2%) vs positive (71.8%) I/O. Negative I/O patients were older with increased comorbidity, pre-existing HF/CKD, acute physiology, IVF volume administration, and diuretic use.Overall, 8,719 patients (15.3%) were readmitted and 3,639 patients (6.4%) died during 30-day post-discharge follow-up. There was no difference in readmission risk between positive vs negative I/O after adjusting for age, sex, race, body mass index, history of CKD/HF, diuretic use, COPS2 (14-15), LAPS2 (14-15), and LOS (HR 1.00, 95% CI, 0.95-1.05). No association was detected between readmission risk and I/O using I/O as continuous, SPLINE, and quadratic function transformations. Table 2 shows adjusted readmission risk by category, with positive I/O associated with lower HF-related readmission risk. Finally, positive I/O was associated with higher adjusted 30-day mortality (HR 1.23, 95% CI, 1.15-1.31, p<0.001).
Conclusions: In this large, multicenter study of non-critically ill sepsis patients, there was no association between positive fluid balance at time of sepsis discharge and readmission risk. Patients with negative fluid balance were older and had higher comorbid disease burden, with increased diuretic use. As a result, the current approach may be vulnerable to residual confounding, and other causal inference or interventional approaches are warranted.