Background: Millions of people are hospitalized in the United States annually and many of those patients are medically complex requiring a team-based approach to care for their medical problems and complex planning for discharge and the transitions thereafter. The process of discharging a patient is multilayered, time-consuming, and arguably one of the most pivotal times during a patient’s hospital stay and most discharges occur in the afternoon to evening hours resulting in bottlenecks. Our group previously assessed barriers to discharge noting that much of the delay for patients who are ready for discharge have their orders delayed because clinicians are caring for other patients. Advanced care providers and multidisciplinary teams may be one way to help relieve this bottleneck such that care can occur in real-time both for patients ready for discharge and those in need of ongoing care. We created a multidisciplinary discharge team that included an Advanced Practice Provider (APP), a pharmacist, and a nurse and sought to understand whether this team could effectively and efficiently prepare discharges while the care team proceeded with other patient care needs.
Methods: A Multidisciplinary Discharge Team coordinated discharge activities for patients ready to discharge including placing discharge orders, conducting discharge medication reconciliation, preparing and reviewing discharge instructions with patient and family, performing any discharge teaching, and arranging relevant post-discharge care. Primary outcomes were: (1) time of day the clinician enters the discharge order, (2) time of day the patient leaves the hospital, and (3) average length of stay. Secondary outcomes are: (1) proportion of patients for whom a discharge order is entered before 11 am, (2) proportion of patients discharged before 11 am, and (3) clinical staff experience collected via REDCap survey.
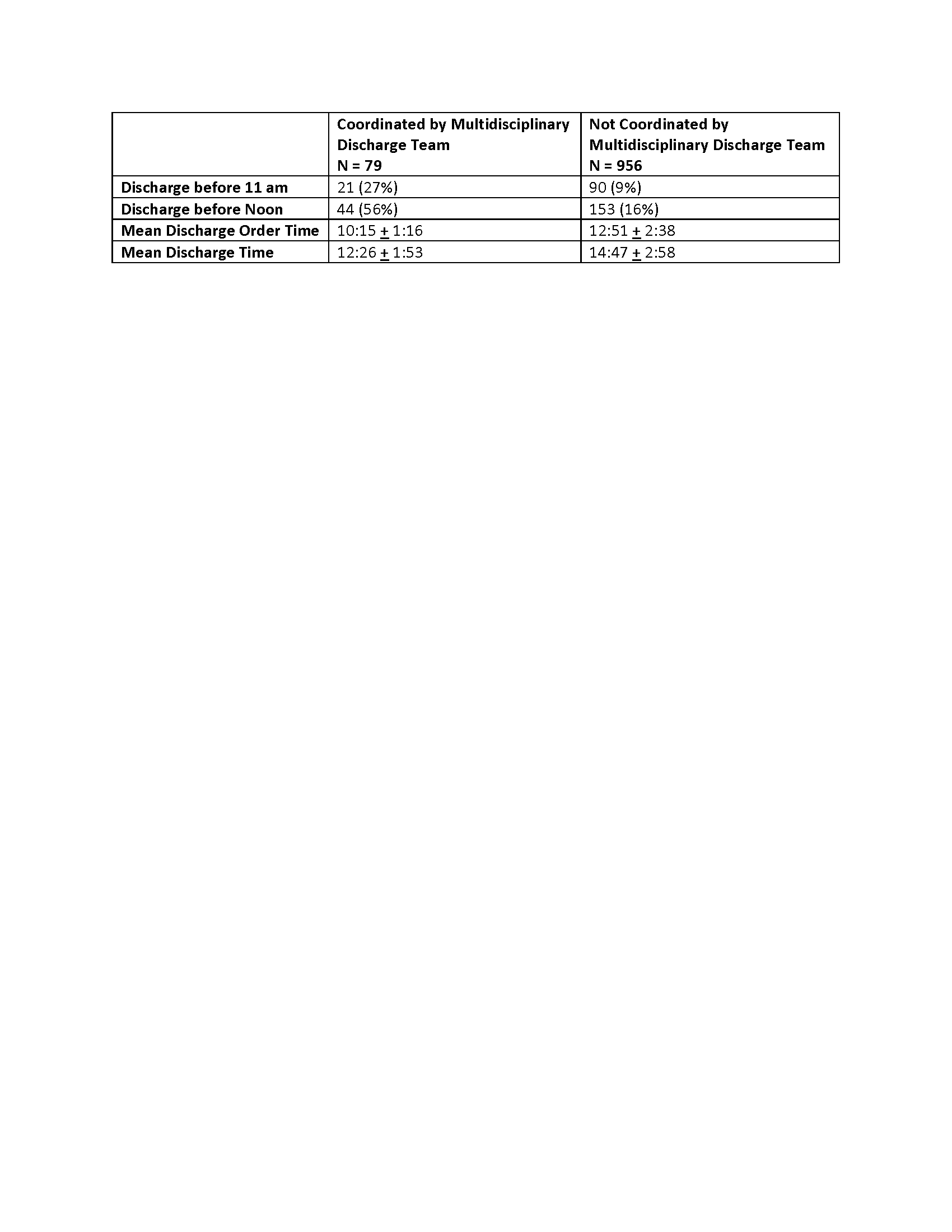
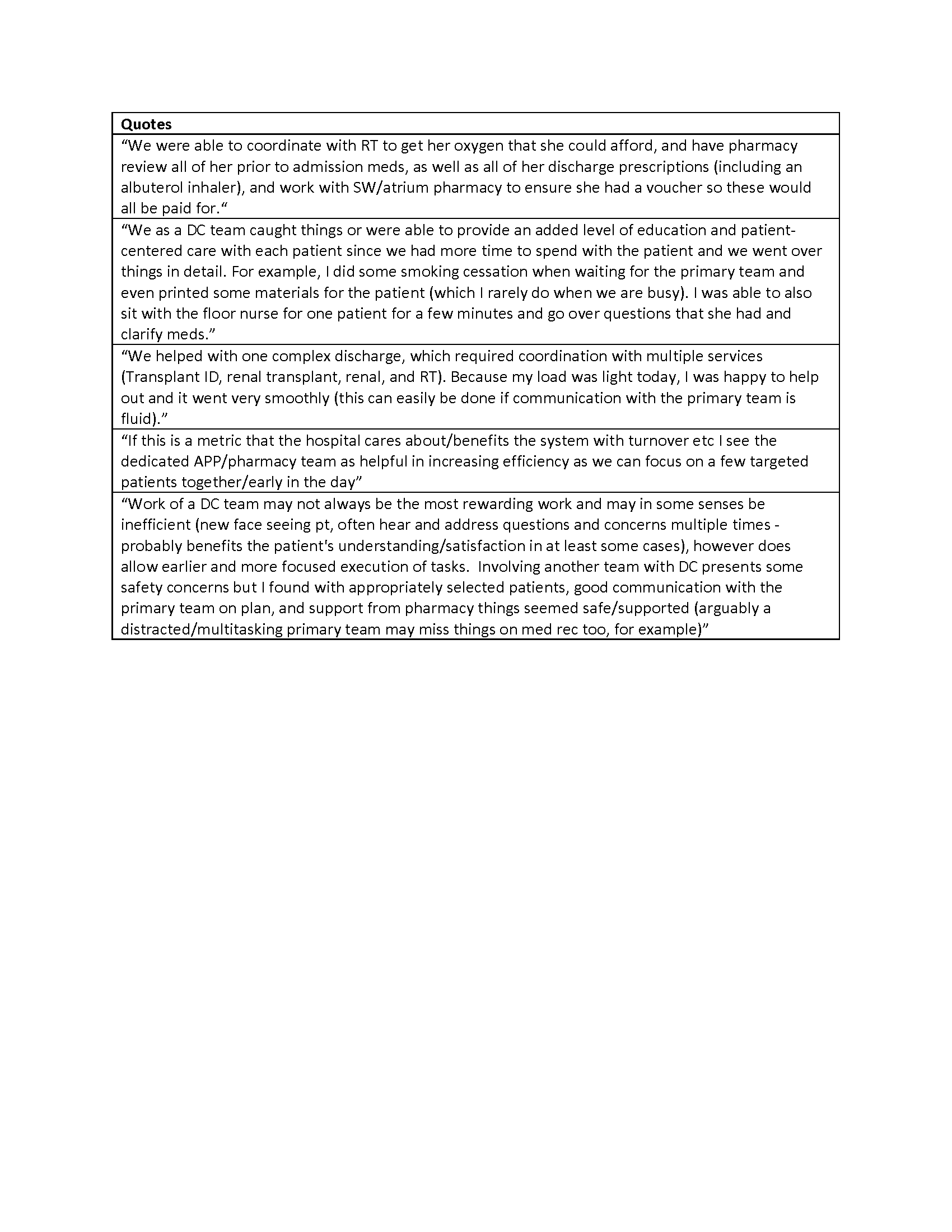
Results: During a six-week pilot test, 87 patients were seen by the Multidisciplinary Discharge Team and of those patients, 79 were discharged on the same day (Table 1). When an APP, nurse, and pharmacist all staffed the discharge team, the delay between discharge order and discharge from the hospital was reduced to an hour and a half. Qualitative data collected from staff working on the Multidisciplinary Discharge Team indicates the team was most effective when an APP, pharmacist, and nurse were all involved (Table 2). Eighty percent of clinical staff who worked with the team and completed a survey would recommend the Multidisciplinary Discharge Team to other providers.
Conclusions: The Multidisciplinary Discharge Team improved discharge times with an overall positive response from providers and staff. Preliminary results suggest this multidisciplinary team may improve efficiency in discharges while allowing teams to provide ongoing care to other patients concurrently.