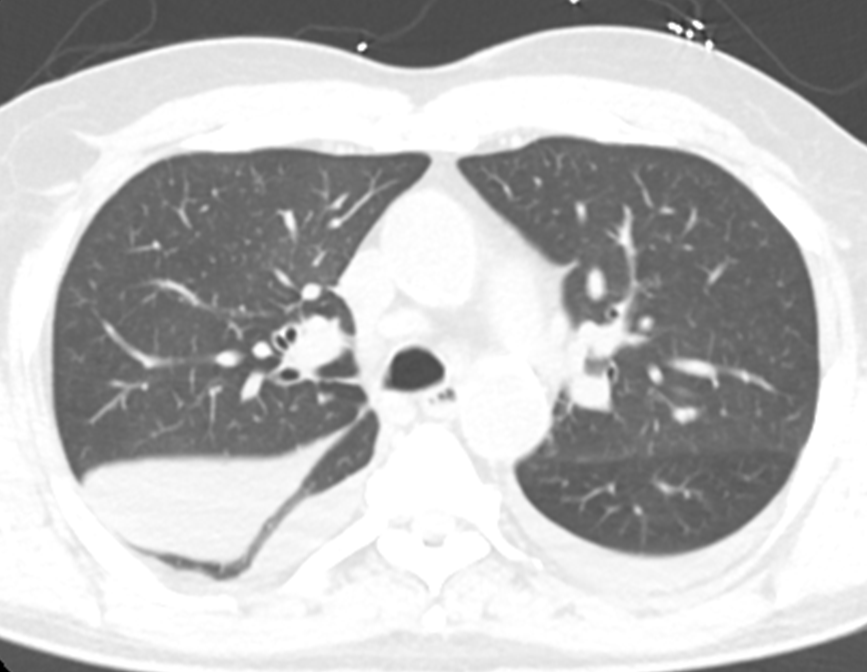
Case Presentation: A 73 year-old man with type 2 diabetes mellitus (hemoglobin A1c 7.5), hypertension, hyperlipidemia, chronic renal failure stage 3a, and a distant 10 pack year smoking history presented with 2 weeks of substernal chest tightness and dyspnea on exertion. He was hemodynamically stable without tachypnea at rest. Examination revealed a grade 2/6 holosystolic murmur at the apex, fine rales over the right lower lung, and 1+ bilateral lower extremity edema. The creatinine was 2.18 mg/dL (baseline creatinine 1.50 mg/dL) and the brain natriuretic peptide level (BNP) was 849 ng/L.Chest X-ray (CXR) demonstrated a large density in the right lower lung field region with mild pulmonary vascular congestion (Figure 1). Lateral CXR suggested location of the density to be in the right middle lobe region. CT Thorax (Figure 2) revealed ground glass opacities in the right perihilar region and an elliptical 7×3 cm fluid collection with a tail that clearly showed it to be located in the right major fissure. Transthoracic echocardiogram (TTE) showed an ejection fraction 60-64% with mitral and tricuspid regurgitation. Left ventricular relaxation was impaired with elevated left ventricular filling pressure.The patient was treated with oral furosemide 20mg daily. Repeat CXR after 3 days showed resolution of the right lung density. Patient was discharged on hospital day 3 with plans for further evaluation of heart function.
Discussion: “Vanishing tumor syndrome” is a well-described but uncommon finding wherein a volume-overloaded patient presents with what appears to be a lung mass but is actually a loculated interlobar pleural effusion, usually in the right minor fissure. The finding most strongly indicative of an intrapleural collection is the way it tails off into a fissure. The diagnosis is confirmed when the “tumor” disappears with correction of volume status. These lesions occur with adhesions and obliteration of the pleural space secondary to earlier pleuritis, thus restricting the free movement of fluid. The location of this patient’s loculated effusion in the right major fissure is uncommon in presentations of vanishing tumor syndrome.This case provides an example of a patient without a known history of congestive heart failure (CHF) who presented with a radiologic finding suggesting a lung mass. The case highlights the importance of harnessing physical examination and laboratory findings to refine the differential diagnosis and guide management, which allowed us to arrive at a diagnosis before undergoing a lengthy and expensive oncologic workup. As with more typical pleural effusions in CHF, this “potential mass” resolved with medical management.
Conclusions: In evaluating a patient with a newly recognized radiologic finding suggesting a lung mass in the setting of symptoms consistent with CHF, careful attention should be taken in assessing for physical exam and lab findings of volume overload. Remembering to keep a loculated pleural effusion on the differential for a patient with a presentation similar to this case can be crucial in avoiding the physical, financial, and emotional cost to the patient of an oncologic workup.