Background: For academic hospital medicine groups to thrive and be partners with their hospital systems, physicians must document and bill appropriately as a means of demonstrating their clinical value. Yet, many major academic hospital medicine groups may be unaware or receive little training for this very important skill set. Based on data from the Society of Hospital Medicine’s State of Hospital Medicine Report from 2018, for groups with 30 or more full time equivalent positions, the responsibility of selecting the correct current procedural terminology (CPT) code lands on the provider 80.3% of the time.
Purpose: Our division created a Billing Best Practices Committee to educate faculty on billing practices to accurately reflect our group’s clinical productivity and to mitigate potential lost revenue.
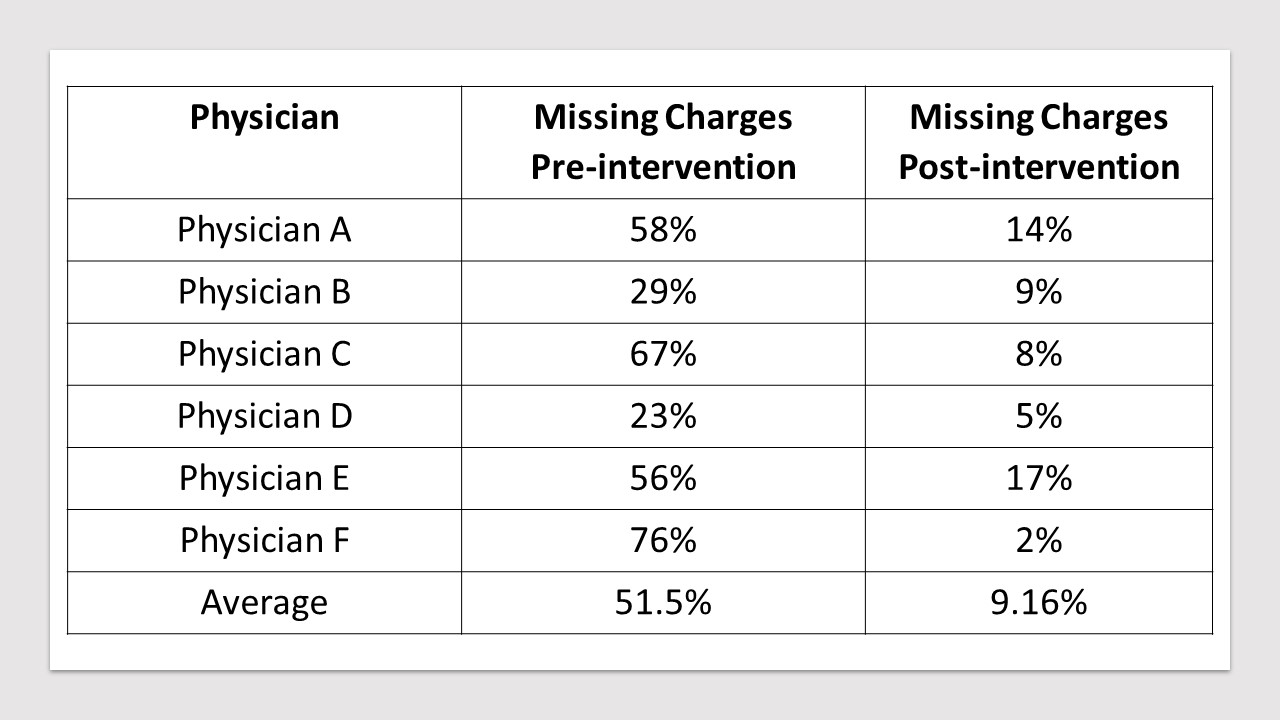
Description: In 2018, we assembled a team and created a framework to ensure that our faculty receive training in clinical documentation and billing. The committee consists of our Division Head, Director of Clinical Operations, Division Administrator, and three other highly clinical faculty. Our mission was to develop a billing curriculum to teach new faculty and audit billing practices of current faculty to minimize lost revenue. After reviewing the billing data for our division, we identified two performance measures to improve upon: rates of missing charges and changed CPT codes. The hospital’s billing department flagged providers with missing charges and changed CPT codes after a secondary review. Changed CPT codes are defined as down charges or up charges based on Centers for Medicare and Medicaid Services documentation requirements. Missing charges means that the provider did not bill for the clinical encounter. Our first aim was to develop a billing curriculum to teach new hires. Starting in academic year 2019, all 14 of our new physician hires received training on billing best practices, including a review of inpatient CPT codes, time-based billing, and billing based on the components of history, physical exam, and medical decision making. New faculty attend three one-hour courses in their first year to reinforce this training and to review their own billing audits. We then tracked the rates of missing charges and changed CPT codes of new hires compared to the rest of the faculty over the year. The rate of missing charges for new hires was 1.96% compared to the remaining faculty at 6.15%. The rate of changed CPT codes was comparable between the two groups with new hires at 5% and remaining faculty at 4.3%. The committee’s secondary goal was to identify established physicians with the highest rates of missing charges and provide feedback on how to improve their compliance rates. This feedback included incorporating billing as part of their daily routine after writing notes and adding a “dropped charges” column to their patient list in the electronic medical record which alerts physicians if they have billed for the day. After this intervention, there was an improvement in this cohort’s rate of missing charges from 51.5% to 9.16%.
Conclusions: Academic hospitalist groups have a mission to provide high quality patient care while advancing education and innovation. One way to demonstrate value within a healthcare system is to appropriately capture productivity for direct patient care. By creating a standardized billing curriculum for new hires and providing continuous feedback, physicians are held accountable to patients and themselves to ensure appropriate and timely billing for the comprehensive services they provide.