Case Presentation: 75 year old with non-alcoholic cirrhosis, heart failure preserved ejection fraction (HFpEF) and recurrent abdominal abscesses presented with platypnea orthodeoxia syndrome (POS) following diuresis. His oxygen saturation was 100% when lying flat and 78-80% when upright. Trans-esophageal echocardiogram confirmed a sinus venosus defect (SVD) with partial anomalous pulmonary venous return (PAPVR) of right upper pulmonary vein (RUPV) to superior vena cava (SVC). Manifestation of POS was attributed to a decrease in left ventricular end diastolic pressure (LVEDP) after treatment of HFpEF and reduced systemic vascular resistance (SVR) in the setting of cirrhosis which resulted in right to left shunting at the SVD with change in position. The patient’s diuretics were decreased and he was started on midodrine to increase SVR. He was high risk for surgical closure therefore was referred for cardiac magnetic resonance imaging (CMR) for pre-procedural planning and transcatheter closure of the defect.
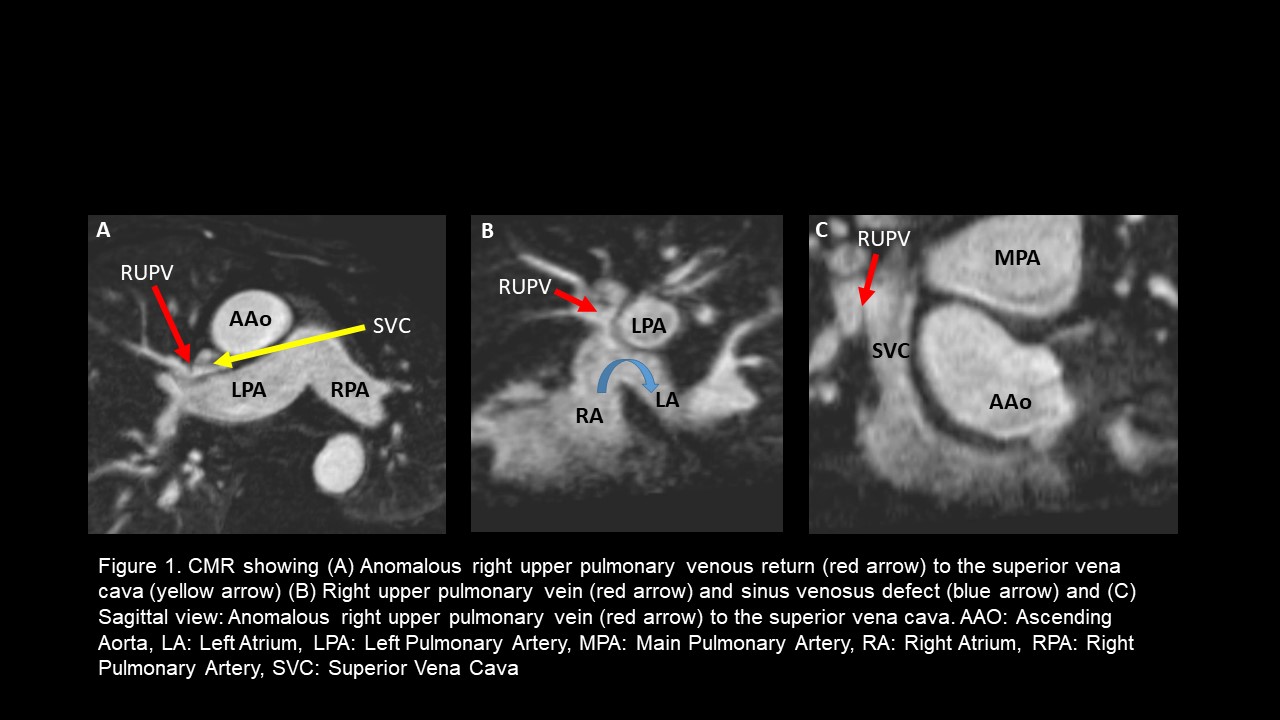
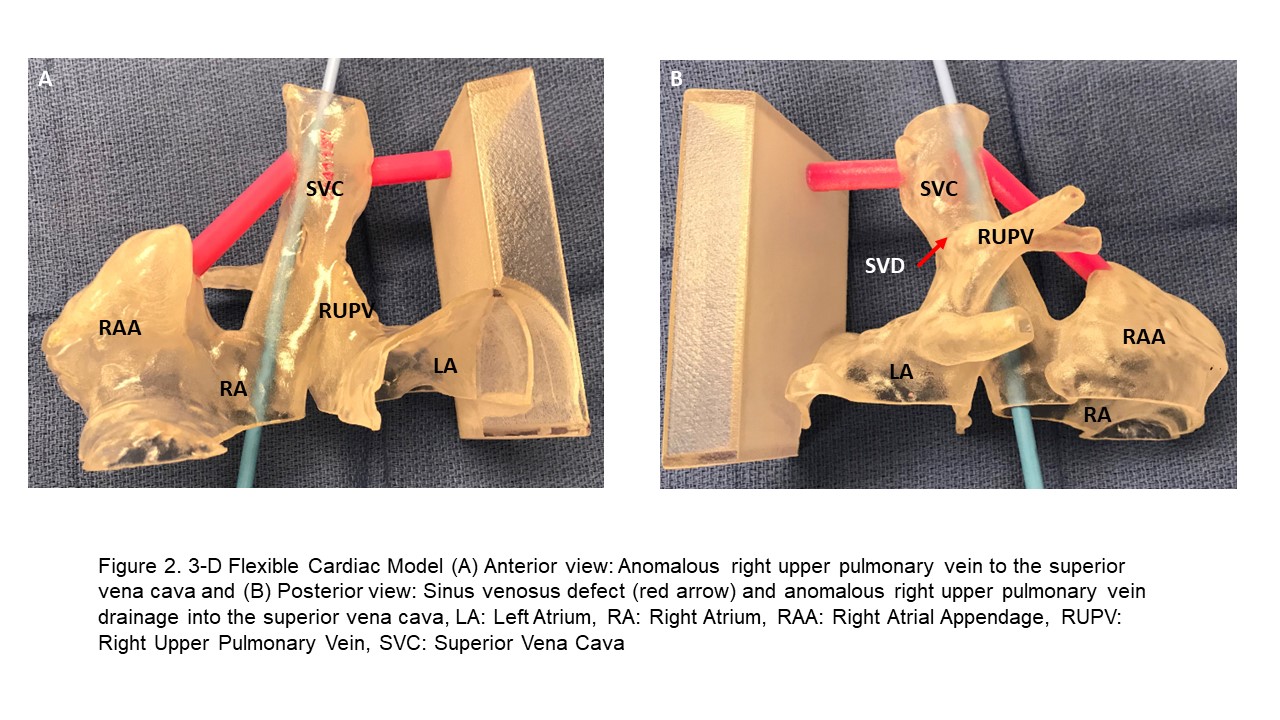
Discussion: CMR showed SVD and PAPVR with RUPV to SVC along with right ventricular volume overload. (Figure 1). CMR was used for 3-dimensional printing of a flexible model with relevant parts of the SVC, right atrium and left atrium to demonstrate the relationship of the SVD and RUPV to the defect itself as well as to right and left atria. The 3D model facilitated procedural planning; goal being to close the SVD without causing pulmonary vein stenosis (Figure 2). The patient underwent cardiac catheterization with two Cheatham Platinum (CP) covered stents delivered via the SVC to close the defect and redirect the RUPV flow into the left atrium. Following the procedure patient had oxygen saturation of 97-100% that did not vary with position.
Conclusions: POS is a rare manifestation of atrial septal defects (ASD). Historically, SVDs have been closed surgically due to the proximity to the SVC, absence of appropriate rims for percutaneous device placement and risk for pulmonary vein obstruction. Based on the CMR derived 3D model we were able to virtually plan stent positioning to close the SVD without impinging on the pulmonary vein ostium. In this case, we used CMR for pre-procedural planning to successfully close the SVD and redirect pulmonary venous flow in the cardiac catheterization laboratory in a symptomatic patient that was high risk for surgical closure.